Lysis of Adhesions (LOA) Doctor

Do you have a stiff knee, or have you been diagnosed with stiff knee syndrome or arthrofibrosis? Arthrofibrosis can occur after knee surgery or after a traumatic injury. Arthroscopic knee surgeon, Doctor Riley J. Williams can treat stiff knee syndrome for patients in Manhattan, Brooklyn, New York City and surrounding areas, using a treatment called lysis of adhesions. This very specialized surgery should be done by an expert. For an evaluation of your knee stiffness and to see if you can be helped by this procedure, contact Dr. Williams’ team today!
What is knee arthroscopy lysis of adhesions (LOA)?
Knee arthroscopy lysis of adhesions is a minimally invasive surgery that uses small incisions and surgical tools to remove scar tissue and tightness in the knee. Lysis of adhesions involves cutting bands of abnormal tissue called adhesions. Scar tissue can form in the knee joint after an injury or prior surgery. Severe cases of scar tissue formation can lead to the development of arthrofibrosis (global knee scarring). Soft tissue adhesion and scar tissue can restrict movement in the joint, cause pain, and limit range of motion. The goal of lysis of adhesions is to restore near normal knee function and kinematics by removed all abnormal soft tissue connections and scar tissue. A deep understanding of knee anatomy and mechanics is necessary to treat knee dysfunction associated with adhesions, scar tissue and arthrofibrosis. Dr. Riley J. Williams, orthopedic knee surgeon, serving Manhattan, Brooklyn, New York City, NY and surrounding areas, has extensive experience in performing knee arthroscopy lysis of adhesions procedures.
Why is knee arthroscopy LOA performed?
Knee arthroscopy lysis of adhesions is performed on individuals who have exhausted conservative treatment methods for knee stiffness or arthrofibrosis (stiff knee syndrome). Knee arthrofibrosis can occur after a traumatic injury or surgery (i.e. ACL reconstruction or knee replacement). Stiff knee syndrome limits mobility because scar tissue entraps the knee joint structures. In this condition, the synovium (joint lining) becomes globally inflamed and thickens as a natural response to trauma. Arthrofibrosis causes muscle and connective tissue in the knee to shorten and stiffen. If physical therapy is unsuccessful in treating knee stiffness, lysis of adhesions (LOA) may be the next step in treatment.
How is knee arthroscopy LOA performed?
Sedation with regional anesthesia is most often used for this procedure. Knee arthroscopy lysis of adhesions uses surgical tools and a small camera called an arthroscope. The knee is inflated with fluid to provide greater space and access within the joint for the procedure. Small incisions are made in the knee which allows for the arthroscope to project images of the injury onto a monitor. Adhesions are identified and then debrided with a surgical device called an arthroscopic shaver. Any areas of abnormal constraint or connection are released. Often an arthroscopic radiofrequency device is used for soft tissue release and vessel cautery during LOA. A lateral retinaculum release may be done as part of an LOA. This means the ligaments on the outer side of the knee are loosened for patients who experience limited patellar (kneecap) mobility. Improved patella mobility and excursion is a major goal of lysis of adhesions. Upon completion of the needed soft tissue releases, the knee is manipulated to confirm increased range of motion and normal stability.
As a note, more severe cases of arthrofibrosis may require a small incision to fully excise all of the scar tissue present. This is a judgment call that is determined by findings at the time of surgery. Fortunately, the need for open surgery does not change the postoperative management of affected patients.
What are the risks of lysis of adhesion surgery?
Knee arthroscopy lysis of adhesions is a simple procedure but the aftercare is important to maximize clinical results. The outcome of the surgery can be highly dependent on how quickly the surgery was performed after the onset of the arthrofibrotic condition. In the most severe cases, full knee range of motion may not be achievable even after surgery. Compliance with physical therapy is crucial to a successful outcome. The patient should expect swelling and soreness temporarily afterward the procedure. Other issues such as infection, bleeding, blood clots and continued stiffness are possible but rare.
How long does it take to recover from lysis of adhesions surgery?
Patients treated with lysis of adhesions go home the day of surgery. Range of motion exercises should be started the day following the procedure; physical therapy starts 3-5 days after surgery and continues 2-3 times per week for approximately eight weeks. After six weeks, improved range of motion and patella excursion should be observed. Pain medications, such as narcotics as well as NSAIDs (non-steroidal anti-inflammatory) medications will be necessary immediately following surgery. Crutches are recommended for the first three days after the procedure for swelling reduction and stability.
For additional resources on knee arthroscopy lysis of adhesions or to have your knee pain evaluated, please contact the office of Dr. Riley J. Williams, MD, orthopedic knee surgeon serving Manhattan, Brooklyn, New York City, NY and surrounding areas.
Knee PVNS Doctor

Have you been diagnosed with PVNS? Pigmented villonodular synovitis or PVNS of the knee is a condition which can cause knee pain and stiffness. If you have PVNS, it is important to see an orthopedic surgeon who specializes in the treatment and care of this rare condition. PVNS surgeon Doctor Riley J. Williams provides diagnosis as well as surgical and nonsurgical treatment options for patients in Manhattan, Brooklyn, New York City and surrounding areas who have been diagnosed with this knee condition. Contact Dr. Williams’ team today!
What is knee arthroscopy removal of PVNS lesions?
Pigmented Villonodular Synovitis (PVNS) is a benign condition of the joint lining (synovium) that can results in mechanical symptoms, pain and inflammation. The knee joint commonly affected by PVNS. Knee arthroscopy to remove a PVNS lesion is a procedure that utilizes small surgical tools, and a camera called an arthroscope to remove the mass and abnormal tissue. The cause of Pigmented villonodular synovitis is unknown. The layer of tissue that lines tendons and joints, most commonly in and around the knee, overgrows, causing a lesion or tumor. PVNS can be diffuse or localized. Diffuse PVNS is more widespread within the joint and more challenging to treat. Surgery for diffuse PVNS involves the use arthroscopic instruments to meticulously remove the damaged synovial (joint) lining. Localized PVNS usually occurs in one area of the joint. PVNS is a challenging knee condition; patient should seek experienced surgeons when dealing with this particular diagnosis. Dr. Riley J. Williams, orthopedic knee surgeon, serving Manhattan, Brooklyn, New York City, NY and surrounding areas, has extensive experience in performing knee arthroscopy removal of PVNS lesion procedures.
Why is knee arthroscopy removal of PVNS lesion performed?
Synovium is the joint lining and produces synovial fluid which lubricates the joint and enables smooth pain free motion. If an individual suffers from PVNS, he or she experiences an excess of synovial fluid, and chronic swelling. The synovium overgrows and thickens. This causes swelling, stiffness, and dysfunction. Knee arthroscopy is used to remove the abnormal synovium and to repair any observed damage. The procedure is done arthroscopically if the PVNS lesion is exists within the knee joint. Arthroscopy is done with the use of small surgical instruments and an arthroscope that projects images of the knee onto a monitor. If the PVNS lesion exists outside of the joint space, an open surgical approach may be necessary to effectively remove the abnormal tissue. Most cases of PVNS occur in the knee but can also afflict other joints. This progressive disease can cause bone damage and arthritis.
How is knee arthroscopy removal of PVNS lesion performed?
Many cases of pigmented villonodular synovitis (PVNS), lesion removal are done arthroscopically. Light sedation with regional anesthesia is typically used in these cases. Dr. Williams makes small incisions around the knee to insert the arthroscope and surgical tools. Images of the knee are displayed on a monitor in the operating room. Dr. Williams assess the entirety of the joint to fully grasp the extent of the disease and to confirm the accuracy of preoperative imaging studies. Arthroscopic tools are used to remove all visually confirmable diseased tissue. Arthroscopic surgery can be performed for both localized and diffuse PVNS.
What are the risks of pigmented villonodular synovitis surgery?
For the treatment of intraarticular disease, knee arthroscopy is preferred when performing removal of PVNS lesions. Risks and complications are still possible with this complicated procedure; open procedures may be needed though in more extensive cases. The goals is the removal of as much of the lesion as possible. An individual may continue to experience pain, stiffness, swelling, limited mobility as well as popping, catching or locking of the knee. Although rare, localized PVNS can come back after surgery. The chance of diffuse PVNS to recur is typically around 10 percent but can be as high as 30 percent.
How long does it take to recover from PVNS surgery?
An individual can expect recovery to take a minimum of six weeks; a full recovery may take several months depending on the severity of PVNS disease. Physical therapy is important to regain mobility and strength in surrounding muscles. Most patients will be able to return to normal sports and activities within a few months of knee arthroscopy with the removal PVNS lesion.
For additional resources on knee arthroscopy with removal of PVNS lesions or to have your knee pain evaluated, please contact the office of Dr. Riley J. Williams, MD, orthopedic knee surgeon serving Manhattan, Brooklyn, New York City, NY and surrounding areas.
Knee Arthroscopy Surgeon

Are you an athlete or active individual who is experiencing pain in, under, or to the side of your kneecap? Do you feel like your patella moves incorrectly, or are you bothered by constant knee pain? If so, you may have a knee condition called anterior knee pain which can be helped by a non-invasive procedure called lateral release. Arthroscopic knee surgeon, Doctor Riley J. Williams provides diagnosis as well as surgical and nonsurgical treatment options for patients in Manhattan, Brooklyn, New York City and surrounding areas who are experiencing knee pain and require a lateral release. Contact Dr. Williams’ team today!
What is knee arthroscopy lateral release?
Arthroscopic lateral release surgery describes a procedure that treats painful condition of the kneecap or patella. Often, the soft tissue structures around the kneecap tighten and contract; in these circumstances, the tracking of the patella is altered which results in anterior knee pain. Release of the soft tissues around the patella can provide substantial pain relief. Typically, the knee retinaculum on the lateral side of the knee is cut to realign of the patella. This procedure enables the patella to glide more efficiently in the trochlear groove. Releasing the retinaculum is helpful for those who suffer from a misalignment of the patella. Dr. Riley J. Williams, orthopedic knee surgeon, serving Manhattan, Brooklyn, New York City, NY and surrounding areas, has extensive experience in performing knee arthroscopy lateral release procedures.
Why is knee arthroscopy lateral release performed?
Individuals who suffer knee pain on the lateral side of the patella may need surgery if conservative treatment methods fail. If nonoperative methods such as knee bracing, rest, activity modification or physical therapy do not provide adequate pain relief, a lateral release may be the next step in treatment to realign the patella. Releases can be done to treat partial dislocations of the kneecap and overload syndromes of the kneecap as well. Partial dislocation can stem from a lateral patellar tilt, lateral riding patella, or both. The strong quad muscle on the outer side of the thigh can pull the patella out of its groove; this is known as a lateral patellar tilt. If an individual’s kneecap rests higher in the thighbone than normal, it can cause dislocation and is referred to as lateral riding patella. Lateral release can allow the patella sit more centrally in the groove. Lateral release can also decrease the load the patella experiences during normal sporting and day to day activities such as stairclimbing, running and squatting.
How is arthroscopic (keyhole) lateral release surgery performed?
This is a minimally invasive arthroscopic procedure that is performed on an outpatient basis. Light sedation and regional anesthesia are used for this procedure. Dr. Williams will begin the surgery by making two small incisions in the knee. These incisions allow the arthroscope and surgical tools to be inserted into the knee. Fluid is used to inflate and expand the knee joint to allow Dr. Williams to properly perform the surgery. Images of the knee joint are projected onto a monitor while Dr. Williams releases the retinaculum. This release decreases the tension that pulls on the patella. Improved side to side patella mobility is typical following lateral retinaculum release. Movement of the kneecap is tested before the incision sites are sutured closed. The patient is typically able to go home shortly after waking up from surgery.
What are the risks of lateral release?
This type of knee arthroscopy is a relatively simple; the risks associated with this procedure are minimal. Care is taken to cauterize all visual bleeding in the knee joint as postoperative blood collection in the knee can occur and cause pain and inflammation. The development of scar tissue and infection is also possible but occur rarely. The best chances of a successful outcome can depend heavily on whether an individual is a good candidate for surgery. Factors such as age, activity level and overall health can play a role. Dr. Williams discusses the risk and benefits with all patients prior to moving ahead with this procedure.
How long does it take to recover from a lateral release?
The vast majority of patients go home shortly after the surgery. Crutches are used the first week. Physical therapy starts approximately one week following surgery, and continues for about 8 weeks. Full recovery is expected between 3-6 months depending on the patient’s ability to regain normal lower extremity strength.
For additional resources on knee arthroscopy lateral release or to have your knee pain evaluated, please contact the office of Dr. Riley J. Williams, MD, orthopedic knee surgeon serving Manhattan, Brooklyn, New York City, NY and surrounding areas.
Knee Cartilage Repair Surgeon

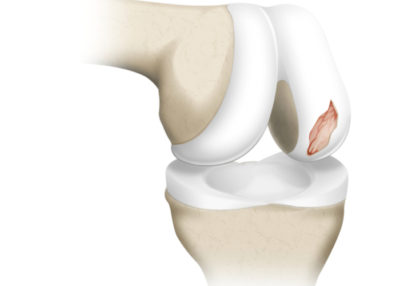
Chondral defects, or articular cartilage defects of the knee can be caused by over-use, a sports injury, or from an accident or traumatic event. Over time, the damaged tissue can wear down to the bone and create a painful condition called osteoarthritis. Articular cartilage repair and restoration surgeon Doctor Riley J. Williams provides diagnosis as well as surgical and nonsurgical treatment options for patients in Manhattan, Brooklyn, New York City and surrounding areas who have sustained an ACL injury. Contact Dr. Williams’ team today!
What is knee chondral or knee cartilage repair and reconstruction?
Most often, cartilage repair and reconstruction describes the surgical treatment of symptomatic articular defects of the knee. Such surgery can also be performed in the ankle, shoulder, hip and elbow. There are many types of cartilage surgery that can be used to treat these chondral lesion or defects. The type of surgery that is indicated is dependent upon the location of the knee cartilage damage. Most of these techniques can be performed arthroscopically or using a small incision to access the damaged area. The goal of cartilage repair and reconstruction is to restore healthy functional cartilage-like tissue to the area of cartilage loss. Successful cartilage repair reduces knee pain, mitigates cartilage degeneration, and restores knee function.
There are several types of repairs or reconstruction surgeries available to affected patients: chondroplasty, mosaicplasty, microfracture, synthetic scaffold cartilage surgery, osteochondral autograft transplant (OAT) osteochondral allograft transplantation, matrix-associated autologous autologous chondrocyte implantation (MACI), and particulate or minced juvenile articular cartilage. Dr. Riley J. Williams, orthopedic knee and joint preservation specialist, serving Manhattan, Brooklyn, New York City, NY and surrounding areas, has extensive experience in cartilage repair and reconstruction surgeries of the knee.
What is cartilage damage?
There are several types of cartilage. Articular cartilage in the knee is a tough, slippery form of connective tissue that acts as a shock absorber within joints. This type of cartilage in the knee covers the ends of the bones and helps the joint to move smoothly and painlessly. Knee articular cartilage can become damaged from normal wear and tear, repetitive overuse, or due to traumatic injury (i.e. patella dislocation, acute ACL tears). Cartilage injury results in a loss of tissue that causes abnormal joint friction; over time, this cartilage erosion results in arthritis. Symptomatic cartilage loss can limit an individual’s ability to participate in sports and activities of daily life. Damaged cartilage does not grow back or heal on its own. Current operative techniques can help restore damaged cartilage.
What is chondroplasty and how is it done?
Chondroplasty is a surgical procedure wherein the area of affected cartilage damage is debrided to facilitate smooth joint motion. Colloquially, chondroplasty can also be termed a “clean out”. This outpatient, arthroscopic surgery is typically used for individuals suffering from mild to moderate cartilage damage; it also commonly used as an in-season treatment strategy for athletes. During chondroplasty, Dr. Williams smooths all areas of cartilage damage, removes loose bodies, and addresses other potential issue such as meniscus tears or synovitis. Adjunct therapies such as platelet rich plasma injection, bone marrow aspirate concentrate (BMAC) or adipose based stromal cells injection may be indicated in conjunction with chondroplasty.
What is microfracture and how is it done?
Microfracture is a procedure wherein small holes are created in the base of a cartilage lesion to promote a healing response and create cartilage repair tissue. The holes that are created in the base of cartilage lesion enable marrow elements (stem cells) to migrate into the area of cartilage damage to support the repair process. Microfracture is used to treat small areas of cartilage damage, typically in the knee. Microfracture typically results in the formation of scar tissue or fibrocartilage that is not as durable or effective as healthy articular cartilage. Microfracture can be performed arthroscopically and is effective for the short-term treatment of knee cartilage defects. In general, more modern techniques are indicated for patients who desire a durable long term solution.
What is matrix associated autologous chondrocyte implantation (MACI) and how is it done?
MACI is a surgical procedure used to treat large areas of damaged cartilage within the knee. The MACI procedure is done with two separate arthroscopic procedures. The first procedure harvests cartilage cells (chondrocytes); these cells are used to create a cartilage scaffold or “patch” that can be used to repair an area of cartilage damage. The second procedure involves the implantation of this seeded scaffold into the damaged area. MACI utilizes a sample of an individual’s own chondrocytes, which are removed from the knee and grown ten times the size in a laboratory for approximately 6-8 weeks. Once the cellular implant is ready, it is placed it over the damaged cartilage area in the knee. The implant is glued in place. The cells and scaffold facilitate the creation of durable cartilage repair tissue.
What is osteochondral autograft transfer (OATS) or autologous osteochondral transfer (AOT) and how is it done?
Osteochondral autograft transfer (OATS) or autologous osteochondral transfer (AOT) are the same procedure. These terms describe an arthroscopic procedure in which a healthy bone-cartilage plug is harvested from an area of the knee that bears minimal weight (usually the central portion of the knee). These healthy bone-cartilage plugs are then transplanted to an area of cartilage damage. Typically, two-four plugs can be harvest and used to treat a symptomatic lesion of the knee condyles, trochlea or patella. Plugs diameters range from 6-10 mm; plug length is usually 10-15 mm. Dr. Williams places these plugs in a manner to fully resurface the area of cartilage damage. The bony base of these plugs heals quickly to the bone of the affected area. There is immediate fill of the defect. Healing occurs quickly over the first 4-6 weeks following implantation. This method is an excellent choice for high demand individuals. The results of autograft osteochondral transfer are very good and durable.
What is autograft or autologous mosaicplasty and how is it done?
Autograft mosaicplasty may also be referred to as an osteochondral autograft transplant (AOT). This type of repair surgery is indicated for high demand individuals or individuals suffering from a small to medium sized articular lesion of the knee (up to 5 cm2) Mosaicplasty is often performed arthroscopically; on occasion a small incision may be necessary Dr. Williams will remove any broken pieces of bone or cartilage during the surgery. Healthy tissue is harvested from a non-weight bearing area of the knee joint. The harvested plugs are used to repair the damaged area. Backfill of the harvested sites is completed using bone from the cartilage lesion or from a donor source (allograft).
The use of several small grafts, instead of one large graft, can help minimize morbidities or undesirable complications, such as misshapen grafts, which can affect smooth knee movement.
What is osteochondral allograft transplantation and how is it done?
Cartilage repair surgery that uses a donor source of cartilage and bone to repair a cartilage defect is termed osteochondral allograft transplantation. In these cases, a donated condyle specimen is used to craft a graft to reconstruct an area of cartilage damage. Typically, one or two cylindrical bone-cartilage grafts are used to restore the damaged cartilage area. These donated grafts are press fit into the defect and immediately reconstruct the injury. The donated specimens are fresh; this means that the transplanted cartilage is viable and able to survive for long periods following implantation. This procedure is often performed using regional anesthesia; a small incision is necessary to implant these large grafts. Osteochondral allograft transplantation is highly effective procedure that is very effective in decreasing pain and increasing functions in patients suffering from large cartilage lesions.
What is particulate (minced) juvenile articular cartilage repair and how is it done?
The implantation of small pieces of juvenile articular cartilage can be used to enable the creation of durable cartilage repair tissue in a chondral defect. This product (known as DeNovo NT, Zimmer) is comprised of viable pieces of articular cartilage from young donors. The surgical procedure is simple. The area of cartilage repair is debrided, and all damaged cartilage is removed. A clear host site is created to enable implantation of the minced pieces. Fibrin glue is used to create an implant or the pieces are laid at the base of the defect and glued into place. There is no invasion of bone or structural compromise of the affected area. This procedure can be done arthroscopically or using a small incision. Knee range of motion is held for a few days to facilitate early cartilage incorporation.
How long does it take to recover from cartilage repair and reconstruction?
Recovery time for cartilage repair and reconstruction varies. Most cartilage repair procedures take approximately 6 months to recover. Chondroplasty is the most time efficient (6-8 weeks). Autograft mosaicplasty or OATS can take 4-6 months. Osteochondral allograft transplantation and juvenile minced cartilage implantation require approximately 6 months. MACI usually takes approximately 6-12 months. Ultimately, clearance for full activities following the above procedures is predicated on the creation of a cartilage repair tissue and the patient’s ability to regain lower extremity muscle strength and fitness. Regardless of the type of surgery, it will be important to follow Dr. Williams’ rehabilitation guidelines, which typically include a period of rest for healing, followed by physical therapy and strength training.
For additional resources on cartilage repair and reconstruction or to have your knee pain evaluated, please contact the office of Dr. Riley J. Williams, orthopedic knee surgeon serving Manhattan, Brooklyn, New York City, NY and surrounding areas.
SC Joint Injury Specialist

Are you an athlete who participates in contact sports such as hockey or football? If so, you may be at risk of sustaining a sternoclavicular (SC) joint injury. SC Joint injuries are usually caused by a direct blow or blunt trauma to the collarbone area of the shoulder. SC joint injury specialist, Doctor Riley J. Williams provides diagnosis as well as surgical and nonsurgical treatment options for patients in Manhattan, Brooklyn, New York City and surrounding areas who have sustained an SC joint injury. Contact Dr. Williams’ team today!
What is a sternoclavicular joint injury?
A sternoclavicular (SC) joint injury describes an injury to the joint between the medial clavicle and sternum of the rib cage (thorax). SC joint injuries can occur following a motor vehicle accident or impact associated with contact sports (football, rugby). SC joints can also sustain damage if the protective cartilage in the joint wears away over time due to osteoarthritis. The SC joint is one of four joints within the shoulder. It is located at the base of the neck where the clavicle (collar bone) connects to the sternum (breastbone). Although an injury to the SC joint is uncommon, it can be a serious injury. SC joint injuries are typically associated with significant external force to the chest and airways. Important nerves and blood vessels lie behind the sternoclavicular joint, making these types of injuries potentially serious. Dr. Riley J. Williams, orthopedic shoulder specialist serving Manhattan, Brooklyn, New York City, NY and surrounding areas has extensive experience in treating sternoclavicular joint injuries and other shoulder related injuries.

What are the symptoms of an SC joint injury?
Osteoarthritis, and trauma can cause injury to the SC joint. The symptoms associated with an SC joint injury include:
- Pain and tenderness
- Swelling
- Bruising
- Inability to move the arm in a full range of motion
- Redness over the joint site
- Pain in other joints (associated with rheumatoid arthritis)
- Clicking or grinding noise when the arm is moved
How is an SC joint injury diagnosed?
Dr. Williams will discuss your medical history with you before performing a physical examination. He will inquire when the pain began and if it is related to a particular accident or injury. During the physical exam, Dr. Williams will check for range of motion, tenderness, bumps, or deformities over the joint and the blood flow in the hands and fingers. Imaging tests will be ordered to ensure a proper diagnosis. These may include x-rays, CT scans or an MRI.
How is an SC joint injury treated?
Non-surgical treatment:
It is possible for this type of injury to be treated non-surgically if none of the structures withing the joint are damaged. Dr. Williams may recommend activity modifications and immobilizing the joint to give it time to heal. If the injury is caused by osteoarthritis or rheumatoid arthritis, corticosteroid injections can provide relief from pain and inflammation. Non-steroidal anti-inflammatory medications can also help manage pain and swelling. If the SC joint injury was sustained from a dislocation, Dr. Williams may perform a closed reduction under anesthesia to manipulate bones back into their proper place.
Surgical treatment:
If an open reduction is necessary, it is done under anesthesia and requires incisions to reposition bones into their original position. If the injury stems from an infection, Dr. Williams will need to open the joint to drain the infection. Antibiotics are required after the procedure. Surgical procedures to fix the injury from osteoarthritis are rare but can be performed if conservative treatment methods have failed to alleviate pain. Surgery for SC joint condition is rare. Dr. Williams will be sure such procedures are necessary prior to their indication.
For more information on a sternoclavicular joint injury and the treatment options available, please contact the office of Riley J. Williams, MD, orthopedic shoulder specialist serving Manhattan, Brooklyn, New York City, NY and surrounding areas.



