Knee Cartilage Repair Surgeon

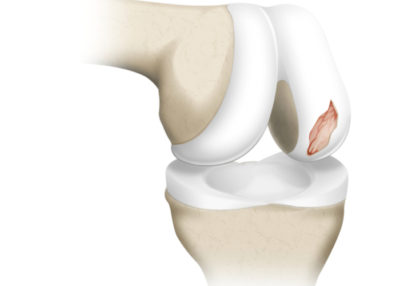
Chondral defects, or articular cartilage defects of the knee can be caused by over-use, a sports injury, or from an accident or traumatic event. Over time, the damaged tissue can wear down to the bone and create a painful condition called osteoarthritis. Articular cartilage repair and restoration surgeon Doctor Riley J. Williams provides diagnosis as well as surgical and nonsurgical treatment options for patients in Manhattan, Brooklyn, New York City and surrounding areas who have sustained an ACL injury. Contact Dr. Williams’ team today!
What is knee chondral or knee cartilage repair and reconstruction?
Most often, cartilage repair and reconstruction describes the surgical treatment of symptomatic articular defects of the knee. Such surgery can also be performed in the ankle, shoulder, hip and elbow. There are many types of cartilage surgery that can be used to treat these chondral lesion or defects. The type of surgery that is indicated is dependent upon the location of the knee cartilage damage. Most of these techniques can be performed arthroscopically or using a small incision to access the damaged area. The goal of cartilage repair and reconstruction is to restore healthy functional cartilage-like tissue to the area of cartilage loss. Successful cartilage repair reduces knee pain, mitigates cartilage degeneration, and restores knee function.
There are several types of repairs or reconstruction surgeries available to affected patients: chondroplasty, mosaicplasty, microfracture, synthetic scaffold cartilage surgery, osteochondral autograft transplant (OAT) osteochondral allograft transplantation, matrix-associated autologous autologous chondrocyte implantation (MACI), and particulate or minced juvenile articular cartilage. Dr. Riley J. Williams, orthopedic knee and joint preservation specialist, serving Manhattan, Brooklyn, New York City, NY and surrounding areas, has extensive experience in cartilage repair and reconstruction surgeries of the knee.
What is cartilage damage?
There are several types of cartilage. Articular cartilage in the knee is a tough, slippery form of connective tissue that acts as a shock absorber within joints. This type of cartilage in the knee covers the ends of the bones and helps the joint to move smoothly and painlessly. Knee articular cartilage can become damaged from normal wear and tear, repetitive overuse, or due to traumatic injury (i.e. patella dislocation, acute ACL tears). Cartilage injury results in a loss of tissue that causes abnormal joint friction; over time, this cartilage erosion results in arthritis. Symptomatic cartilage loss can limit an individual’s ability to participate in sports and activities of daily life. Damaged cartilage does not grow back or heal on its own. Current operative techniques can help restore damaged cartilage.
What is chondroplasty and how is it done?
Chondroplasty is a surgical procedure wherein the area of affected cartilage damage is debrided to facilitate smooth joint motion. Colloquially, chondroplasty can also be termed a “clean out”. This outpatient, arthroscopic surgery is typically used for individuals suffering from mild to moderate cartilage damage; it also commonly used as an in-season treatment strategy for athletes. During chondroplasty, Dr. Williams smooths all areas of cartilage damage, removes loose bodies, and addresses other potential issue such as meniscus tears or synovitis. Adjunct therapies such as platelet rich plasma injection, bone marrow aspirate concentrate (BMAC) or adipose based stromal cells injection may be indicated in conjunction with chondroplasty.
What is microfracture and how is it done?
Microfracture is a procedure wherein small holes are created in the base of a cartilage lesion to promote a healing response and create cartilage repair tissue. The holes that are created in the base of cartilage lesion enable marrow elements (stem cells) to migrate into the area of cartilage damage to support the repair process. Microfracture is used to treat small areas of cartilage damage, typically in the knee. Microfracture typically results in the formation of scar tissue or fibrocartilage that is not as durable or effective as healthy articular cartilage. Microfracture can be performed arthroscopically and is effective for the short-term treatment of knee cartilage defects. In general, more modern techniques are indicated for patients who desire a durable long term solution.
What is matrix associated autologous chondrocyte implantation (MACI) and how is it done?
MACI is a surgical procedure used to treat large areas of damaged cartilage within the knee. The MACI procedure is done with two separate arthroscopic procedures. The first procedure harvests cartilage cells (chondrocytes); these cells are used to create a cartilage scaffold or “patch” that can be used to repair an area of cartilage damage. The second procedure involves the implantation of this seeded scaffold into the damaged area. MACI utilizes a sample of an individual’s own chondrocytes, which are removed from the knee and grown ten times the size in a laboratory for approximately 6-8 weeks. Once the cellular implant is ready, it is placed it over the damaged cartilage area in the knee. The implant is glued in place. The cells and scaffold facilitate the creation of durable cartilage repair tissue.
What is osteochondral autograft transfer (OATS) or autologous osteochondral transfer (AOT) and how is it done?
Osteochondral autograft transfer (OATS) or autologous osteochondral transfer (AOT) are the same procedure. These terms describe an arthroscopic procedure in which a healthy bone-cartilage plug is harvested from an area of the knee that bears minimal weight (usually the central portion of the knee). These healthy bone-cartilage plugs are then transplanted to an area of cartilage damage. Typically, two-four plugs can be harvest and used to treat a symptomatic lesion of the knee condyles, trochlea or patella. Plugs diameters range from 6-10 mm; plug length is usually 10-15 mm. Dr. Williams places these plugs in a manner to fully resurface the area of cartilage damage. The bony base of these plugs heals quickly to the bone of the affected area. There is immediate fill of the defect. Healing occurs quickly over the first 4-6 weeks following implantation. This method is an excellent choice for high demand individuals. The results of autograft osteochondral transfer are very good and durable.
What is autograft or autologous mosaicplasty and how is it done?
Autograft mosaicplasty may also be referred to as an osteochondral autograft transplant (AOT). This type of repair surgery is indicated for high demand individuals or individuals suffering from a small to medium sized articular lesion of the knee (up to 5 cm2) Mosaicplasty is often performed arthroscopically; on occasion a small incision may be necessary Dr. Williams will remove any broken pieces of bone or cartilage during the surgery. Healthy tissue is harvested from a non-weight bearing area of the knee joint. The harvested plugs are used to repair the damaged area. Backfill of the harvested sites is completed using bone from the cartilage lesion or from a donor source (allograft).
The use of several small grafts, instead of one large graft, can help minimize morbidities or undesirable complications, such as misshapen grafts, which can affect smooth knee movement.
What is osteochondral allograft transplantation and how is it done?
Cartilage repair surgery that uses a donor source of cartilage and bone to repair a cartilage defect is termed osteochondral allograft transplantation. In these cases, a donated condyle specimen is used to craft a graft to reconstruct an area of cartilage damage. Typically, one or two cylindrical bone-cartilage grafts are used to restore the damaged cartilage area. These donated grafts are press fit into the defect and immediately reconstruct the injury. The donated specimens are fresh; this means that the transplanted cartilage is viable and able to survive for long periods following implantation. This procedure is often performed using regional anesthesia; a small incision is necessary to implant these large grafts. Osteochondral allograft transplantation is highly effective procedure that is very effective in decreasing pain and increasing functions in patients suffering from large cartilage lesions.
What is particulate (minced) juvenile articular cartilage repair and how is it done?
The implantation of small pieces of juvenile articular cartilage can be used to enable the creation of durable cartilage repair tissue in a chondral defect. This product (known as DeNovo NT, Zimmer) is comprised of viable pieces of articular cartilage from young donors. The surgical procedure is simple. The area of cartilage repair is debrided, and all damaged cartilage is removed. A clear host site is created to enable implantation of the minced pieces. Fibrin glue is used to create an implant or the pieces are laid at the base of the defect and glued into place. There is no invasion of bone or structural compromise of the affected area. This procedure can be done arthroscopically or using a small incision. Knee range of motion is held for a few days to facilitate early cartilage incorporation.
How long does it take to recover from cartilage repair and reconstruction?
Recovery time for cartilage repair and reconstruction varies. Most cartilage repair procedures take approximately 6 months to recover. Chondroplasty is the most time efficient (6-8 weeks). Autograft mosaicplasty or OATS can take 4-6 months. Osteochondral allograft transplantation and juvenile minced cartilage implantation require approximately 6 months. MACI usually takes approximately 6-12 months. Ultimately, clearance for full activities following the above procedures is predicated on the creation of a cartilage repair tissue and the patient’s ability to regain lower extremity muscle strength and fitness. Regardless of the type of surgery, it will be important to follow Dr. Williams’ rehabilitation guidelines, which typically include a period of rest for healing, followed by physical therapy and strength training.
For additional resources on cartilage repair and reconstruction or to have your knee pain evaluated, please contact the office of Dr. Riley J. Williams, orthopedic knee surgeon serving Manhattan, Brooklyn, New York City, NY and surrounding areas.