UCL – MCL Injury Specialist

Are you an athlete or that participates in repetitive overhead motions like baseball, raquet sports or other throwing activities? If so, you may be at risk of sustaining an elbow injury to the ulnar collateral ligament, or UCL. Injury to the ULC or MCL ligament can cause elbow instability, pain and swelling. ULC/MCL specialist, Doctor Riley J. Williams provides diagnosis as well as surgical and nonsurgical treatment options for patients in Manhattan, Brooklyn, New York City and surrounding areas who have sustained an injury to the ULC or MCL in the elbow. Contact Dr. Williams’ team today!
What is an ulnar collateral ligament (UCL) injury?
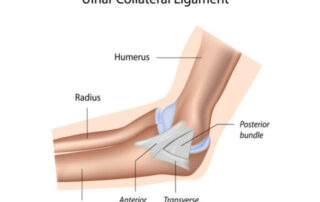
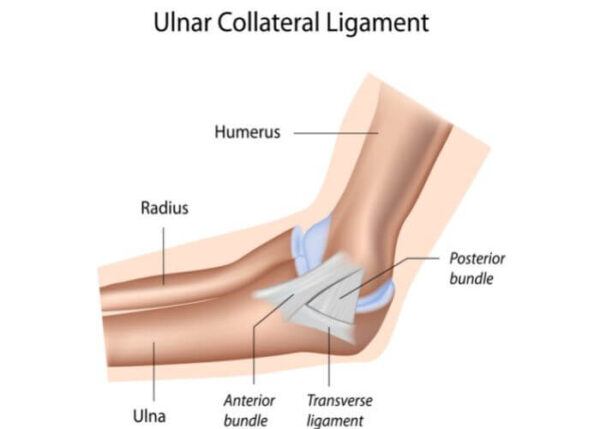
The ulnar collateral ligament (UCL) is a band of thick, fibrous tissue, connecting the humerus (upper arm bone) to the ulna (forearm bone on the medial side). The UCL is also known as the medial collateral ligament (MCL). The UCL is responsible for elbow stability. The UCL is most commonly injured by repetitive overhead throwing or from a traumatic injury. A fall on an outstretched arm can injure the UCL and result in an unstable elbow. The ulnar collateral ligament is divided into three bands of tissue: posterior, anterior and transverse. Injuries to these structures can result in elbow pain, instability, and dysfunction. Dr. Riley J. Williams, orthopedic elbow specialist serving Manhattan, Brooklyn, New York City, NY and surrounding areas has extensive experience in treating ulnar collateral ligament injuries.
What are the symptoms of a UCL injury?
If the injury is chronic, daily tasks will most likely still be manageable. An acute injury will greatly limit functionality, especially if an elbow dislocation has occurred concomitantly. Individuals in the New York area often report the following symptoms for their UCL injury/tear:
- Elbow joint instability
- Pain on the inside of the elbow, exacerbated by overhead throwing
- Elbow swelling
- Weakness
- Popping sound (acute injury)
- Tingling sensation in the pinky finger
- Decreased velocity while throwing or serving
How is a UCL injury diagnosed?
Dr. Williams will discuss the patient’s history and symptoms. He will also perform a physical examination of the arm, elbow, and shoulder. The valgus stress test is a common method to determine elbow instability and to determine the degree of UCL injury.
Dr. Williams uses MRI to confirm and classify the UCL tear. Radiographs are also helpful to rule out related bone injuries. CT scans are sometimes used if severe bony abnormalities are suspected. If related ulnar nerve symptoms are suspected, an EMG and nerve conduction studies may be ordered to rule out cubital tunnel syndrome.
What are the grades of a ulnar collateral ligament (UCL) tear?
Ulnar collateral ligament tears are separated into grades, depending on the severity of the tear:
- Grade 1 tear: The ligament is strained, but not notably stretched. This grade causes pain, but the elbow still functions.
- Grade 2 tear: The ligament is stretched or partially torn, but still is attached at the native insertions on the humerus and ulna.
- Grade 3: The ligament is fully torn or ruptured.
How is a UCL injury treated?
Non-surgical treatment:
If a patient sustains a first or second-degree tear, Dr. Williams may recommend a conservative treatment option of RICE: rest, ice, compression and elevation of the elbow. NSAIDs, such as ibuprofen helps to mitigate pain and swelling. Other options may include splinting the elbow to help ensure rest and proper healing followed by physical therapy, which can strengthen the muscles around the ligament. Platelet rich plasma (blood spin procedure) injections can be of some value in treating partial UCL tears; usually multiple injections are indicated followed by a period of complete rest. In general, nonoperative treatment strategies are very unpredictable for UCL tears.
Surgical treatment:
If a complete or near-complete UCL tear occurs, surgical repair is recommended. Once the UCL is repaired, complete recovery takes approximately 9-12 months. Ulnar collateral reconstruction, also known as Tommy John Surgery, utilizes a tendon from another area in of the patient’s replace the native injured UCL. This procedure is effective at returning high demand athletes to sports.
For more information on a ULC injury and the treatment options available, please contact the office of Riley J. Williams, MD, orthopedic elbow specialist serving Manhattan, Brooklyn, New York City, NY and surrounding areas.
Elbow Nerve Specialist

Are you experiencing pain, tingling, and a “falling asleep” or numb sensation in the little finger and ring finger? If so, you may have ulnar nerve entrapment, or a pinched nerve in your elbow. Also called cubital tunnel syndrome, ulnar nerve entrapment can occur in several places along the nerve path of the arm. Most symptoms are felt on the inside of the elbow and extend to the fingers of the hand. It is very important to visit a doctor at the onset of ulnar nerve compression symptoms to avoid muscle wasting. Ulnar nerve entrapment specialist, Doctor Riley J. Williams provides diagnosis as well as surgical and nonsurgical treatment options for patients in Manhattan, Brooklyn, New York City and surrounding areas who are experiencing the symptoms of a compressed or pinched elbow nerve. Contact Dr. Williams’ team today!
What is ulnar nerve entrapment?
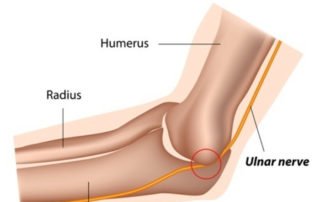
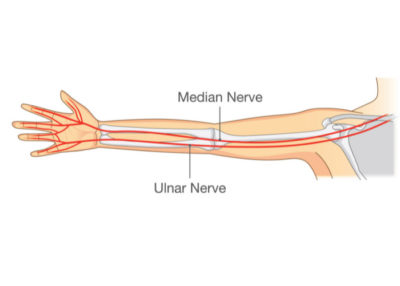
The ulnar nerve is one of three main nerves of the arm. The ulnar nerve runs through the length of the arm and carries signals from the brain to the fourth and fifth fingers of the hand. This nerve courses from the base of the neck, along the inside of the arm, through the elbow and down to the fingers. Ulnar nerve entrapment is also known as cubital tunnel syndrome. An entrapped nerve is clinically the same as a pinched nerve. Entrapment of the ulnar nerve in the cubital tunnel of the elbow causes achiness, pain, tingling and numbness in the forearm and fingers. If left untreated, cubital tunnel syndrome can cause muscle loss in the hand and forearm. The site where the ulnar nerve
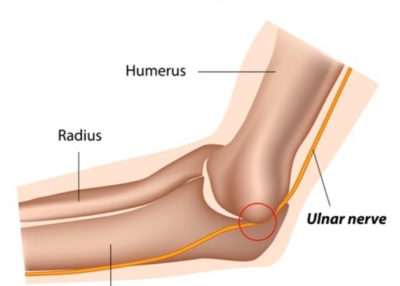
passes through the elbow (cubital tunnel) is narrow; the base of the tunnel is the bony portion of the medial epicondyle of the distal humerus. When the elbow is flexed, the ulnar nerve is stretched and compressed in the cubital tunnel, elbow extension reliefs this tension on the nerve. Though the cubital tunnel is the most common area of ulnar nerve entrapment in the arm, the nerve may be constricted in other areas of the arm as well.
What is cubital tunnel syndrome?
Cubital tunnel syndrome is ulnar nerve entrapment at the site of the medial epicondyle. The cubital tunnel is narrow and is comprised of a bony base and an inflexible ligamentous sleeve. The ulnar nerve travels behind the medial epicondyle in the cubital tunnel. Constriction of the ulnar nerve in the cubital tunnel typically is exacerbated by elbow flexion or bending. Cubital tunnel syndrome can result in pain, numbness and tingling in the forearm, hand and fingers; more severe cases can result in a loss of general motor function in the hand. Dr. Riley J. Williams, orthopedic elbow specialist serving Manhattan, Brooklyn, New York City, NY and surrounding areas has extensive experience in cubital tunnel syndrome and ulnar nerve entrapment.
What are the symptoms of cubital tunnel syndrome?
Individuals in the New York area who suffer from ulnar nerve entrapment or cubital tunnel syndrome often report the following symptoms:
- Forearm, hand and finger numbness and tingling
- Loss of motor skills in the hand
- Loss of dexterity
- Pinky and ring finger tingling/numbness
- Hand clumsiness
- Inability to hold things, resulting in dropping objects
- Worsening symptoms at night, stemming from sleeping in a flexed elbow position
- Pain or a burning feeling in the elbow or funny bone (inner elbow)
How is ulnar nerve entrapment/cubital tunnel syndrome diagnosed?
Dr. Williams performs a physical exam to check for tenderness, motor strength, and sensory changes in the hand, forearm and elbow. Longstanding cases of ulnar nerve can present with muscle distal to the elbow. A diagnostic test, such as an electromyogram (EMG) will demonstrate the functionality of the ulnar nerve and determine where nerve compression may be located.
How is cubital tunnel syndrome treated?
Non-surgical treatment:
Conservative methods are typically the first line of treatment for the ulnar nerve compression. Rest, elbow splints, and NSAIDs, such as ibuprofen, can help reduce pain and inflammation. Physical therapy may be implemented to strengthen the arm muscles; occupational therapy can fine tune motor skills.
Surgical treatment:
If nonoperative methods fail or if cubital tunnel syndrome symptoms are longstanding, surgery is indicated. Dr. Williams performs ulnar nerve decompression and transposition on an outpatient basis. Light sedation and regional anesthetic are used during this surgery. An incision is made at the medial elbow, and the nerve is mobilized and cleared of all adhesions. The nerve can be left in the decompressed tunnel, or moved to a new location that is usually anterior to the cubital tunnel. It typically takes six weeks to recover from ulnar nerve compression surgery.
For more information on ulnar nerve entrapment, cubital tunnel syndrome and the treatment options available, please contact the office of Riley J. Williams, MD, orthopedic elbow specialist serving Manhattan, Brooklyn, New York City, NY and surrounding areas.
Snapping Scapula Specialist

Are you experiencing a snapping sensation in the shoulder blade? Do you have pain along the shoulder blade when moving? If so, you may have a shoulder condition called snapping scapula syndrome. This can be caused by overuse, reaching overhead or by sports that involve overhead movements. Snapping scapula syndrome specialist, Doctor Riley J. Williams provides diagnosis as well as surgical and nonsurgical treatment options for patients in Manhattan, Brooklyn, New York City and surrounding areas who are experiencing snapping scapula syndrome. Contact Dr. Williams’ team today!
What is snapping scapula syndrome?
Snapping scapula syndrome is also known as scapulothoracic bursitis; this malady is characterized by snapping, popping, and pain in the upper back area, usually deep to the shoulder blade. The scapula is the shoulder blade; the scapula is a triangular shaped bone that sits at the superior area of the right and left upper back. A bursa (fluid filled sac) is located between the scapula and the thorax (rib cage). The bursa provide cushioning and protection against friction during movement of the shoulder blade relative to the rib cage. This fluid sac is known as the scapulothoracic bursa. Inflammation of the scapulothoracic bursa can occur is association with weightlifting, throwing, swimming, tennis and a number of other upper extremity based activities. Inflammation of this bursa is also known as scapulothoracic bursitis. Dr. Riley J. Williams, orthopedic shoulder specialist serving Manhattan, Brooklyn, New York City, NY and surrounding areas has extensive experience in treating snapping scapula syndrome and other shoulder related injuries.

What are the symptoms of scapulothoracic bursitis?
The scapula is connected to the rib cage by soft tissue attachments only. There is no bony joint between the thorax and the scapula. These soft tissue attachments allow for the smooth movement of the upper extremity relative to the thorax. Typically, the scapula moves synchronously with the rib cage; inflammation of the deep bursa of the scapula can alter this dynamic. The symptoms of the snapping scapula include:
- Snapping sensation and noises in the shoulder blade
- Swelling
- Stiffness
- Shoulder weakness/instability
- Shoulder blade pain upon movement
- Pain/tenderness
- Noticeable posture difference
- Inability to perform overhead arm movements
How is snapping scapula diagnosed?
Dr. Williams will discuss your medical history and source of pain. He will also perform a physical examination while looking for deformities of the scapula and posture. A physical pop can be detected deeply at the shoulder blade in more severe cases. Shoulder range of motion and strength are assessed. Imaging tests, such as an x-ray, MRI or CT scan can help further diagnose the injury. CT scans are very helpful in detecting deep bony projection of the scapula that may be responsible for this malady.
How is snapping scapula treated?
Non-surgical treatment:
Non-surgical approaches are commonly applied with patients suffering scapulothoracic bursitis. Resting, activity modification and icing the affected area helps to decrease pain and inflammation. Over-the-counter non-steroidal anti-inflammatory medications, such as ibuprofen or naproxen can also help decrease swelling and pain. Range of motion exercises and physical therapy restore normal shoulder motion and motor strength. A strong shoulder girdle helps to improve shoulder kinematics. Dr. Williams may also suggest a corticosteroid injection. These injections provide immediate relief but should be considered carefully prior to adminstration.
Surgical treatment:
If pain, mechanical symptoms and shoulder dysfunction persist after the application of nonoperative treatment strategies, Dr. Williams may recommend surgery. The surgical approach involves removing the scapulothoracic bursa and/or partial scapular resection. A bursectomy is a procedure that removes inflamed bursa and surrounding scar tissue. In addition, irregular bony projections or spurs are typically removed during this procedure. A partial scapular resection focuses on the upper medial portion of the scapula which may be causing improper friction against the thorax (rib cage). Patients are typically immobilized for a few days following this procedure; a sling is used for approximately one week. Physical therapy is started after the first week and typically continues for 2-3 months.
For more information on snapping scapula syndrome and the treatment options available, please contact the office of Riley J. Williams, MD, orthopedic shoulder specialist serving Manhattan, Brooklyn, New York City, NY and surrounding areas.
Ulnar Nerve Transposition Surgeon

Are you experiencing tingling or numbness in the elbow, wrist, or fingers and specifically in the ring and pinky fingers. If so, you may have cubital tunnel syndrome, or a nerve that is pinched in your elbow. This elbow condition can be treated by a procedure called ulnar nerve transposition. Ulnar nerve transposition surgeon, Doctor Riley J. Williams provides diagnosis as well as surgical and nonsurgical treatment options for patients in Manhattan, Brooklyn, New York City and surrounding areas who are experiencing a pinched nerve in their elbow or cubital tunnel syndrome. Contact Dr. Williams’ team today!
What is ulnar nerve transposition?
Ulnar nerve transposition is an outpatient surgical procedure that treats ulnar nerve entrapment or cubital tunnel syndrome. The procedure involves moving the ulnar nerve (“the funny bone”), which runs at from top of the inner upper arm near the shoulder, across the inside of the elbow, and down to the fingers. The ulnar nerve is repositioned from its placement behind the medial epicondyle to an area above the condyle where it will not be compressed or stretched during normal elbow bending. Dr. Riley J. Williams, orthopedic elbow surgeon, serving Manhattan, Brooklyn, New York City, NY and surrounding areas, has extensive experience in successfully performing ulnar nerve transposition procedures.
What is ulnar nerve entrapment?
Ulnar nerve entrapment or compression may also be referred to as cubital tunnel syndrome. Ulnar nerve entrapment is responsible for tingling or numbness in the elbow, wrist, or fingers, specifically the ring and pinky fingers. This long nerve pass through a narrow soft tissue sleeve at the bottom of the medial elbow and is called the cubital tunnel. The nerve run behind the elbow and is stretched when the elbow is flexed or bent. Abnormal constriction or tension of the nerve in the cubital tunnel can lead to pain, numbness and tingling in the forearm and hand. Surgery may be necessary if the numbness and tingling substantially affect hand and finger motor skills.
How is ulnar nerve transposition performed?
Dr. Williams makes an incision by the medial epicondyle; he then carefully locates and exposes the ulnar nerve. A release of the nerve and neurolysis is performed. He then reposition the nerve to a different (more anterior) location on the inside of the elbow. The new placement will be superficial (subfascial), or within the muscle (submuscular). This relocation prevents the nerve from getting stretched or compressed in the cubital tunnel. Following the transposition, the nerve slackens with elbow flexion. Once surgery is completed, the elbow is placed in a bulky dressing and sling for about one week.
What are the risks of ulnar nerve transposition?
Risks from surgery may include:
- Infection
- Continued tingling due to incomplete decompression of the nerve
- Pain at the incision site
- Nausea, vomiting and/or constipation from prescribed pain medication
- Swelling
How long does it take to recover from cubital tunnel surgery?
A bulky dressing is used for about one week after surgery. Physical therapy begins 5-7 days after surgery and patients are encouraged to move their elbow right away. Prescribed pain medication (narcotics) may be advised for a finite period of time after the surgery to stay on top of pain before transitioning to an over-the-counter non-steroidal anti-inflammatory medication PT is recommended to restore mobility, strength and range of motion in the elbow, hand and fingers. Patients can increase their activity to tolerance once the wound is healed and range of motion is restored. A full recovery is expected over 2-4 months.
For additional resources on ulnar nerve transposition or to have your elbow pain evaluated, please contact the office of Dr. Riley J. Williams, MD, orthopedic elbow surgeon serving Manhattan, Brooklyn, New York City, NY and surrounding areas.
Osteochondral Allograft Transplantation Specialist

Dr. Riley J. Williams performed the first fresh osteochondral allograft transplant in New York State in 1998 and since then, has performed over 3,000 OCA transplant surgeries. OCA or osteochondral allograft transplantation treats patients who have large areas of damaged articular cartilage in the knee. If you experience pain, inflammation or catching of the knee that affects your athletic performance or everyday tasks, and if you are under the age of 50, you may benefit from this type of treatment. Patients in Manhattan, Brooklyn, New York City and surrounding areas who would like more information on an OCA transplant should contact Dr. Williams’ team today!
What is osteochondral allograft transplantation (OCA)?
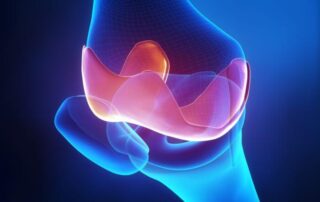
Dr. Williams performed the first fresh osteochondral allograft transplant in New York State in 1998. Osteochondral allograft transplantation is a surgical procedure that uses healthy tissue from a cadaver donor to repair a cartilage injury or defect. Most osteochondral allograft procedures are performed in the knee. Damaged knee articular cartilage results in exposed bone in the knee joint. Loading of this exposed bone causes knee joint pain, friction and inflammation. During an osteochondral allograft transplantation procedure, a donor cartilage graft is shaped to fit the area of cartilage deficit. The allograft is then transplanted into the cartilage defect and replaces the damaged section. The transplanted graft immediately fills in the missing cartilage and help provide the patient with pain relief and improved knee function. Dr. Riley J. Williams, orthopedic knee surgeon, serving Manhattan, Brooklyn, New York City, NY and surrounding areas, has extensive experience in performing osteochondral allograft transplantation.

What does an OCA transplant treat?
Osteochondral allograft transplantation is used to treat large areas of damaged articular cartilage in the knee. If an individual experiences pain, inflammation or catching of the knee that affects athletic performance or everyday tasks, and the individual is under the age of 50, he or she may benefit from this type of treatment. Those who suffer from osteochondritis dissecans (damaged cartilage associated with a bone disorder), avascular necrosis (bone tissue death) or localized, full-thickness cartilage, may benefit from osteochondral allograft transplantation. Osteochondral allograft procedures can be used to treat all surfaces of the knee joint: femur, patella and trochlea. Dr. Williams will discuss the severity of the injury and the required treatment with the patient.
How is an osteochondral allograft (OCA) transplant performed?
Osteochondral allograft transplant is a relatively simple procedure that is done on an outpatient basis. Light sedation and regional anesthesia is used for this surgery. Because Dr. Williams is replacing large areas of cartilage, osteochondral allograft transplantation requires the use of a small incision just adjacent to the patella tendon. Most implanted allografts are cylindrical and are called dowel grafts; the top of the graft is cartilage and the bottom in bone. After Dr. Williams makes the incision, he measures the defect. He prepares the damaged cartilage area in preparation for allograft implantation. The sterile allograft is sized to fit perfectly over the damaged section that was prepared. Most graft are placed as a “press fit”; screws or pins are not typically needed to stabilize these grafts. Graft stability is ensured by bony ingrowth into the base of the implanted graft. Long term graft survival is maintained by the live cells that reside within the cartilage of the donated graft.
Patients use crutches for one week, and then are allowed to full-weight bear. A small brace is used early during the rehabilitation process; bracing discontinued after approximately 3 weeks. Physical therapy starts one week after surgery and continues for about 3 months following the procedure.
What are the risks of OCA surgery?
Rare side effects include infection, bleeding, continued pain, stiffness and allograft rejection. Infection is rare due to strict standards for screening and sterilizing donor tissue; prophylactic antibiotics are always used before surgery to mitigate the infection risk. Larger allografts can fragment or collapse if not properly implanted. Graft rejection is exceedingly rare. Dr. Williams has performed over 3000 OCA procedures and seen this occur in one patient over 20+ years.
How long does it take to recover from an osteochondral allograft transplant?
Most OCA transplant patients are fully recovered around six months. Normal activities of daily living are manageable in most patients by 4 weeks after surgery. Full clearance for sports is predicated on the return of normal knee strength, range of motion and coordination. MRI scans are used at 6 months to confirm graft incorporation and competency prior to clearance for sports.
For additional resources on osteochondral allograft transplantation or to have your knee pain evaluated, please contact the office of Dr. Riley J. Williams, MD, orthopedic knee surgeon serving Manhattan, Brooklyn, New York City, NY and surrounding areas.