Patella Cartilage Injury Specialist

Are you experiencing knee pain and swelling with activity? Does your knee lock or feel like it might “give way?” If so, you may have a patellar chondral defect. The protective cartilage of the patella, or kneecap an become damaged from a prior injury, or from wear-and-tear. Patellar chondral defects can eventually lead to osteoarthritis. Patellar defect specialist, Doctor Riley J. Williams provides diagnosis as well as surgical and nonsurgical treatment options for patients in Manhattan, Brooklyn, New York City and surrounding areas who are experiencing symptoms of a patellar chondral defect or lesion. Contact Dr. Williams’ team today!
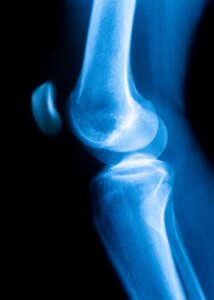
What is the patella?
The patella, or the kneecap, is a small, flat, moveable bone that protects the knee joint. This bone is held in place by the quadriceps tendon and the patellar tendon. The femur (thigh bone), tibia (shin bone), and patella (kneecap) form the knee joint, and are covered by articular cartilage. Articular cartilage facilitates the smooth articulation of these bones during walking, bending, or running. Articular cartilage is a white, slick, tissue found on the ends of the bones; cartilage the “gristle” on the end of a chicken bone.
What is a patellar chondral defect?
A patellar cartilage or chondral defect occurs when the articular cartilage that lines the patella become damaged. The damaged cartilage prevents the knee bones from sliding together smoothly. Articular cartilage is a type of tough, slippery tissue that covers the ends of bones and joint cavities and provides a cushion. Cartilage helps to both protect vulnerable bone ends, and to prevent the bones from grinding together. This cartilage can be damaged in a few different ways: long-term wear, a traumatic injury, or a disorder of the bone. Over time, as the bones move and rub together, the articular cartilage can wear down and begin to expose the surface of the bone. A sudden twist or blow to the knee can also cause a patellar chondral defect by directly damaging the articular cartilage. Dr. Riley J. Williams, orthopedic knee specialist, diagnoses and treats patients with patella chondral and cartilage defects in Manhattan, Brooklyn, New York City, NY and surrounding areas.
How severe is a patellar chondral defect?
Patellar chondral defects range in severity from patient to patient. These defects or injuries are typically graded on a scale from 1-4 to categorize the severity of the damage to the articular cartilage.
- Grade 1: Softening or slight indentation of the cartilage.
- Grade 2: Small partial thickness lesions or fragmentation of the cartilage.
- Grade 3: Larger and deeper lesions or fragmentation of the cartilage.
- Grade 4: Full erosion of the cartilage resulting in exposed bone.
What is a patellar chondral lesion?
A patellar chondral lesion is a type of damage to the articular cartilage of the knee. Patellar chondral lesions most often occur from a traumatic injury to the knee, such as sudden pivot or knee dislocation. However, patellar chondral lesions may occur due to wear-and-tear sustained over time. If left untreated, these defects can ultimately result in arthritis in the knee and frequent pain. Chondral lesions and condral defects are similar; they both describe damage to the articular cartilage.
What are the symptoms associated with patellar chondral defects or lesions?
Symptoms typically noted with the presence of a patellar chondral defect include:
- Anterior knee pain with prolonged or intense activity.
- Swelling or stiffness of the knee.
- Knee instability — knee “buckling”, giving way, giving out, the knee is unable to support your weight.
- Noise during movement — The knee may audibly creak or have a grating sound while walking.
- Locking or catching of the knee.
How are patellar chondral defects diagnosed?
To diagnose patellar chondral defects, Dr. Williams will perform a physical examination of the knee; he will also collect a history of the patient’s activity levels and recent injuries. The physical exam will assess for swelling, decreased range of motion, and the stability of the joint. It can be difficult to diagnose this type of injury, so Dr. Williams may use imaging to further analyze the knee. X-rays can show the space between the femur and kneecap: typically, with patellar chondral defects, this space is narrowed. An MRI will reveal damage or defects in the articular cartilage. Finally, Dr. Williams may perform an arthroscopic exam, which is a minimally invasive surgical technique to view the patella and surrounding tissues. A small incision is created, allowing for an arthroscope (small camera) to be inserted into the knee joint to visualize the joint structures.
Can patellar chondral defects be treated without surgery?
Although there are many surgical techniques to treat patellar chondral defects, there are several non-operative approaches that patients can pursue to treat this condition. Oftentimes, weight loss is suggested to reduce the stress placed on the knee joint. Physical therapy is another great option. Physical therapy can help to increase knee range of motion, promote the lower extremity strengthening, and decrease knee swelling. Articular cartilage cannot heal itself or regrow. However, increasing leg muscles strength can reduce the pain and damage caused by the lack of cartilage. Medications such as NSAIDs (non-steroid anti-inflammatory drugs) are also often prescribed for pain relief.
In some cases, patella chondral defects cause great pain and severely reduce mobility to a degree that non-operative measures are not effective. In such circumstances, surgery it typically recommended as a means of helping patients return to their normal activities. Dr. Williams may perform one of the following surgical procedures:
- Joint arthroscopy with debridement
- Osteochondral autograft transplantation (mosaicplasty)
- Osteochondral Allograft Transplantation
- Particulate Juvenile Articular Cartilage Implantation
- Autologous Chondrocyte Implantation (ACI)
- Tibial tubercle osteotomy
For more information about patellar chondral defects or patellar chondral lesions or for additional resources regarding kneecap cartilage injuries and the treatment options available, please contact the office of Riley J. Williams, MD, orthopedic knee specialist serving Manhattan, Brooklyn, New York City, NY and surrounding areas.
Locations
610 W 58th Street
New York, NY 10019
148 39th Street, 7th Floor
Brooklyn, NY 11232