Shoulder Joint Resurfacing Surgeon

Do you have severe shoulder pain and loss of strength and range of motion associated with degenerative joint disease or arthritis? Have conservative measures failed to alleviate your shoulder pain? If so, you may be a candidate for a type of reconstructive shoulder surgery called shoulder joint resurfacing. The goal of shoulder resurfacing is to avoid a total shoulder replacement, by resurfacing the bone of the shoulder joint. Shoulder joint resurfacing surgeon, Doctor Riley J. Williams provides diagnosis as well as surgical options for patients in Manhattan, Brooklyn, New York City and surrounding areas who have advanced shoulder arthritis and degenerative joint disease. Contact Dr. Williams’ team today!
What is shoulder arthritis?
The glenohumeral joint of the shoulder is where the head of the humerus (upper arm bone) and the glenoid socket of the scapula (shoulder blade) come together. Articular cartilage lines the ends of these bones within the shoulder joint. Cartilage is a slippery white connective tissue that surrounds the ends of bones and facilitates painlessly bone on bone motion within joint movement. Shoulder arthritis is characterized by cartilage loss or damage; loss of the articular cartilage leads to painful bone-on-bone joint movement. There are many types of arthritis; each type of arthritic condition has a unique cause. Osteoarthritis is also known as wear and tear arthritis. Osteoarthritis typically occurs because of repetitive loads across a joint surface. Osteoarthritis can occur as part of the aging process, usually affects individuals over the age of 50. Autoimmune conditions (rheumatoid arthritis, psoriatic arthritis) can also result in shoulder arthritis. In these conditions, the body’s own immune system attacks and destroys the joint cartilage; the shoulder joint can be affected by rheumatoid and psoriatic arthritis. Post-traumatic arthritis occurs following a traumatic injury such as a fracture or dislocation. Shoulder arthritis, when left untreated, can cause chronic shoulder pain, joint damage, and, in some cases, loss of movement.
What is the treatment for shoulder arthritis?
Individuals with mild to moderate shoulder dysfunction associated with degenerative joint disease may benefit from conservative therapy alone. Rest, activity modification, the application of ice and heat, and non-steroidal anti-inflammatory medications (NSAIDs) can be used to control pain and decrease inflammation. Corticosteroid injections can be administered if the pain and inflammation are not relieved with oral medications. A physical rehabilitation program may also be helpful to affected patients by improving shoulder girdle strength and range of motion.
Individuals with severe shoulder pain and dysfunction associated with degenerative joint disease, and those patients who fail conservative measures, are best treated with reconstructive shoulder surgery. The goal of shoulder arthritis surgery is to resurface the bone of the glenohumeral or shoulder joint. Shoulder resurfacing or replacement surgery decreases pain, and restores function, strength, and range of motion. Total shoulder replacement has been the “gold standard” for the treatment of shoulder arthritis for many decades. Less intrusive methods of treating shoulder arthritis have been developed over the past several years, and include shoulder resurfacing. The shoulder resurfacing technique involves removing only the diseased portion of the shoulder joint and is less invasive than total shoulder replacement.
What is shoulder joint resurfacing?
Shoulder joint resurfacing is effective for the treatment of osteoarthritis or rheumatoid arthritis; this surgical procedure is also indicated for other shoulder conditions such as rotator cuff arthropathy, post-traumatic arthritis, and avascular necrosis. Shoulder resurfacing replaces the damaged surfaces of the shoulder with prosthetics designed to restore the natural curvature and glide of the joint. Doctor Riley J. Williams, orthopedic shoulder surgeon, treats patients in Manhattan, Brooklyn, New York City, NY and surrounding areas, who have experienced shoulder arthritis and need surgical treatment.
How is shoulder joint resurfacing performed?
Dr. Williams evaluates several key factors, such as the patient’s age, medical history, and desired outcome, to determine if the patient is a good candidate for shoulder joint resurfacing. This procedure is typically done on an outpatient basis using a combination of sedation, and regional anesthesia. Once positioned, a traditional anterior incision (delto-pectoral) and approach is used to access the joint and perform the surgery.
Shoulder joint resurfacing is performed on the humeral head and the glenoid socket of the scapula. The humeral head is resurfaced using specialized surgical instruments that remove and cover the damaged area. The humeral head is prepared to receive the hemispheric, metallic implant; most the proximal humeral humerus is left intact. For the glenoid, a high molecular weight dense plastic prosthesis is used to reconstruct the shoulder socket.
What are the advantages of shoulder joint resurfacing?
Dr. Williams is a proponent of shoulder joint resurfacing in the appropriate circumstances. Shoulder joint resurfacing is less disruptive to the local shoulder anatomy and requires minimal bony resection. Shoulder joint resurfacing patients should expect clinical outcomes that are equal to more traditional total shoulder replacement techniques.
What is the recovery period like after shoulder joint resurfacing?
Most patients can expect a return to normal daily activities approximately 3-4 weeks after shoulder joint resurfacing. In general, patients in New York can typically anticipate:
- Same day discharge home after the procedure or an overnight hospital stay.
- Joint immobilization using a sling for 2 weeks. Shoulder movement exercises are encouraged immediately after surgery. The sling is used to allow muscle-tendon healing following the resurfacing procedure. Heavy lifting is discouraged during the early stages of recovery.
- Post-surgical pain and inflammation are controlled with a combination of rest, ice, and non-steroidal anti-inflammatory medications (NSAIDs). Dr. Williams may prescribe stronger pain medication to be taken as directed.
- The key to a successful recovery following shoulder joint resurfacing is adhering to and completing the physical rehabilitation program designed by Dr. Williams. The physical therapy program will be aimed at improving the mobility and strength of the shoulder muscles. Physical therapy typically lasts 2-3 months following the shoulder resurfacing procedure.
For more information on shoulder joint resurfacing, or to discuss your shoulder osteoarthritis treatment options, please contact the office of Riley J. Williams, MD, orthopedic shoulder doctor at the Hospital for Special Surgery (HSS), serving Manhattan, Brooklyn, New York City, NY and surrounding areas.
Nerve Entrapment Specialist

Are you an athlete who participates in sports that invovle repetetive overhead movements like swimming, volleyball, baseball or tennis? If so, you may be at risk of developing a pinched nerve in your shoulder called suprascapular nerve entrapment. This condition can cause upper back and shoulder pain and even loss of shoulder function. Shoulder nerve entrapment specialist, Doctor Riley J. Williams provides diagnosis as well as surgical and nonsurgical treatment options for patients in Manhattan, Brooklyn, New York City and surrounding areas who have suprascapular nerve entrapment, or a compressed nerve in their shoulder. Contact Dr. Williams’ team today!
What is suprascapular nerve entrapment?
The suprascapular nerve arises from the middle of the cervical spine and innervates the supraspinatus and infraspinatus muscles of the rotator cuff. This nerve provides both motor and sensory information to these muscles in order to stabilize arm movements that occur at the shoulder joint. Suprascapular nerve entrapment, also known as suprascapular neuropathy, is a condition that results from impingement or damage to the suprascapular nerve. Conditions that are associated with suprascapular neuropathy include: rotator cuff tears, shoulder dislocation, fractured scapula fractures (shoulder blade), clavicle (collarbone) fractures, nerve stretch injuries, direct shoulder trauma, stab wounds and gunshot injuries. The patient with suprascapular nerve entrapment usually presents with shoulder pain and weakness. The signs of suprascapular neuropathy overlap with other more common shoulder conditions; this rare condition can often be overlooked or misdiagnosed. If suprascapular nerve entrapment is suspected, it is important to seek immediate medical attention from a medical professional or orthopedic shoulder specialist to prevent further damage to the suprascapular nerve. Dr. Riley J. Williams, orthopedic shoulder specialist serving patients in Manhattan, Brooklyn, New York City, NY and surrounding areas, has the knowledge and understanding, as well as substantial experience, in treating patients who have experienced suprascapular nerve entrapment.

What is suprascapular nerve compression?
Suprascapular nerve compression occurs when another anatomic structure presses directly on the nerve. Such structures include local ligaments (i.e. the suprascapular ligament) that can thicken and trap the suprascapular nerve. The nerve is also commonly entrapped at the spinoglenoid notch as it passes through to the infraspinatus muscle. Tumors, ganglion cysts, labral cysts and other structural irregularities of the scapula can cause suprascapular nerve compression.
Are there certain populations at greater risk for suprascapular nerve entrapment?
Yes. Since repetitive stretching of the suprascapular nerve can result in suprascapular neuropathy, athletes who consistently perform repetitive overhead movements (volleyball, baseball, weightlifting, swimming, tennis) are at high risk of developing suprascapular nerve entrapment. However, individuals with certain underlying health conditions that lead to the weakening of the scapular muscles, abnormal bone development, or scapular ligament irregularities are also at an increased risk for developing suprascapular nerve entrapment.
What are the symptoms of suprascapular nerve entrapment?
A common complaint of suprascapular neuropathy is a burning pain that radiates to the affected arm, neck, or back. Other symptoms of suprascapular nerve entrapment include:
- Shoulder pain, upper back discomfort
- Pain that generally worsens with shoulder movement
- Weakness of the affected shoulder or arm, especially external rotation of the arm
- Atrophy or deterioration of the affected shoulder muscles
- Partial or complete loss of shoulder function
How is suprascapular nerve entrapment diagnosed?
Because the symptoms of suprascapular neuropathy overlap with common shoulder conditions, it is important to seek prompt medical attention from an orthopedic shoulder specialist familiar with this condition. Dr. Williams will obtain a comprehensive medical history and perform a thorough physical examination. Specialized diagnostic imaging will be obtained to confirm damage to the suprascapular nerve. These imaging techniques may include radiographs, ultrasound, electromyography/nerve conduction study, and magnetic resonance imaging (MRI).
What is the treatment for suprascapular nerve entrapment?
Non-surgical treatment:
If a diagnosis of suprascapular nerve entrapment is confirmed, and the symptoms do not interfere with activities of daily living, conservative therapies may be sufficient in treating this condition. A combination of rest, ice, and non-steroidal anti-inflammatory medications (NSAIDs) are encouraged to control pain and to fdecrease inflammation. Applying heat prior to any shoulder stretching or strengthening activities is also recommended. Physical therapy aimed at increasing mobility, strength, and range of motion of the shoulder is recommended.
Surgical treatment:
In the event of severe nerve compromise, or if conservative therapy was unsuccessful, Dr. Williams may recommend an arthroscopic procedure to decompress the suprascapular nerve. Once the area of nerve compression is identified, Dr. Williams is able to expose the area and relieve the local nerve compression using minimally invasive instrumentation. This minimally invasive surgical approach is an effective technique for suprascapular nerve decompression. The arthroscopic approach shortens the recovery time for patients to return to their normal daily and athletic activities.
For more information on suprascapular nerve entrapment, or the excellent treatment options available, please contact the office of Dr. Riley J. Williams, an orthopedic shoulder specialist serving Manhattan, Brooklyn, New York City, NY and surrounding areas.
Pectoralis Major Tendon Repair Surgeon

A pectoralis major tendon injury occurs when the tendon is pulled away from its attachment site on the humerus (upper arm bone). Pectoralis major tears are often seen among individuals involved in weight-lifting and labor-intensive work. While a partially torn tendon or a tendon strain can be treated conservatively, completely torn pectoralis major tendons require surgery. Pectoral tendon surgeon, Doctor Riley J. Williams provides diagnosis as well as surgical and nonsurgical treatment options for patients in Manhattan, Brooklyn, New York City and surrounding areas who have sustained a pectoralis major tendon injury. Contact Dr. Williams’ team today!
What is a pectoralis major tendon injury?
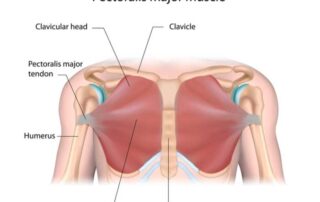
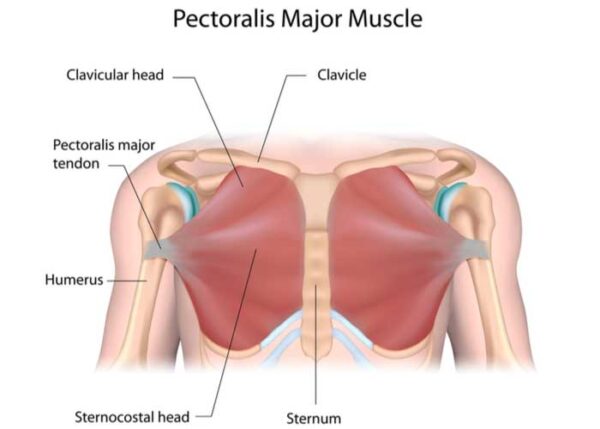
Located on the anterior (front) chest wall are two large, fan-shaped muscles. These muscles are part of the pectoral major complex and are also known as the “pecs”. The pectoralis major muscle originates from the center of the sternum (chest) and clavicle (collarbone). The muscle travels along the chest wall where it ultimately anchors to the humerus (upper arm bone) by means of the pectoralis major tendon. The pectoralis minor muscle originates from the third, fourth, and fifth ribs and attaches to the coracoid process of the scapula (shoulder blade). These muscles work in concert to provide strength and stability to the shoulder when lifting or pushing heavy objects. A pectoralis major tendon injury occurs when the tendon is pulled away from its attachment site on the humerus. Pectoralis major tears are often seen among individuals involved in weight-lifting and labor-intensive work. This type of injury results when the force applied to the pectoralis major muscle exceeds the strength of the pectoralis major tendon’s attachment to the humeral bone. A partial tendon tear may only affect the sternal head of the pectoralis major tendon, whereas a complete tendon tear involves both the sternal head and the clavicular head of the pectoralis major.
What is the treatment for a pectoralis major tendon injury?
A pectoralis major tendon strain, partial tendon tear, or muscle strain/tear can generally be treated conservatively. Patients are encouraged to decrease or avoid activities that initially caused the injury or exacerbate the pain. A combination of rest, ice, and non-steroidal anti-inflammatory medications (NSAIDs) is also recommended for pain management.
Most pectoralis major tendon injuries will require surgery to repair the tendon. Surgical intervention is the most reliably successful method for repairing a pectoralis major tendon injury. Surgical repair of the tendon involves reattaching the tendon to its the correct anatomical position on the humerus. The goal of surgically repairing a pectoralis major tendon injury is to restore stability and strength to the shoulder. A chronically torn pectoralis tendon is a debilitating condition. Dr. Riley J. Williams, orthopedic shoulder doctor, treats patients in Manhattan, Brooklyn, New York City, NY and surrounding areas, who have experienced a pectoralis major tendon injury and need a surgical repair.
How is a pectoralis major tendon repair performed?
Pectoralis major tendon repair requires a small incision near the native insertion of the tendon on the humerus. Prior to the procedure, the patient is placed under light sedation and regional anesthesia is administered. A small incision is made over the anterior shoulder. The dissection localized and identifies the torn tendon edge. After removing the devitalized tissue on the lateral margin of the torn tendon, it then reattached to the humerus using strong sutures and anchors that are placed within the humeral bone.
Patients who present with a chronically torn pectoralis major tendon may experience shortening or scarring. In these circumstances, a tendon graft, either from the patient (autograft) or a donor (allograft), may be necessary to facilitate the proper reattachment of the tendon to the humeral shaft. This tendon graft is then sewn into the native pectoralis major muscle prior to bony reattachment. To prevent pectoralis major tendon retraction and scarring, patients who have experienced a pectoralis major tendon tear are strongly encouraged to seek immediate medical attention as these can make for a difficult surgical repair.
What is the recovery period like after a pectoralis major tendon repair?
The recovery period following a pectoralis major tendon repair is dependent on the injury severity and chronicity. Most patients can expect a return to normal daily activities in approximately 6 weeks. A full recovery, including sports, typically takes 4-6 months. In general, patients in New York can expect the following:
- Immobilization of the shoulder joint, with a sling or other device, immediately following surgery and remain immobilized for 2 weeks.
- A combination of rest, ice, and non-steroidal anti-inflammatory medications (NSAIDs) will be used to control pain and decrease inflammation. Dr. Williams may prescribe stronger pain medication to be taken as directed.
- Active participation and completion of the physical rehabilitation program detailed by Dr. Williams is the key to a successful recovery. Passive and active shoulder exercises are carefully performed with the help of the physical therapy team to re-establish shoulder strength, mobility, and range of motion. Formal PT starts one week after surgery and continue for approximately 3 months.
For more information on pectoralis major tendon repair, or to discuss your pectoralis major tendon treatment options, please contact the office of Riley J. Williams, MD, orthopedic shoulder doctor at the Hospital for Special Surgery (HSS), serving Manhattan, Brooklyn, New York City, NY and surrounding areas.
Clavicle Fracture Specialist

A clavicle or collar bone fracture can occur from a fall, trauma, work injury or from a direct blow, experienced during work or a sports collision. Common symptoms of a fractured clavicle include sharp pain at the time of injury and difficulty with pain when moving the arm. Collar bone fracture specialist Doctor Riley J. Williams provides diagnosis as well as surgical and nonsurgical treatment options for patients in Manhattan, Brooklyn, New York City and surrounding areas who have sustained a clavicle injury or broken collarbone. Contact Dr. Williams’ team today!
What is a clavicle fracture?
The clavicle (collarbone) is a long s-shaped bone that connects the upper limb to the thorax. Together, the clavicle and the scapula (shoulder blade) form the shoulder girdle. The clavicle is often broken when the shoulder experiences trauma such as a direct blow or a fall onto an outstretched arm. Clavicle fractures are common, and account for 5% of all adult bone fractures. Dr. Riley J. Williams, orthopedic shoulder specialist serving patients in Manhattan, Brooklyn, New York City, NY and surrounding areas, has the knowledge and understanding, as well as substantial experience, in treating patients who have experienced a clavicle fracture.

Are there different types of clavicle fractures?
Classification of clavicle fractures is based on the anatomical location of the fracture, as follows:
- The fractured portion of the clavicle occurs in the middle of the bone; this area is the most common location of a break. If the bones remain in the correct anatomical position with minimal displacement, midshaft fractures can be treated without surgery.
- Lateral/Distal. The fractured portion of the clavicle occurs at the point furthest away from the body’s midline near the top of the scapula. Surgery may be necessary depending on the location of the fracture and the associated bony displacement.
- The fractured portion of the clavicle occurs at the point closest to the neck. These fractures are rare and account for approximately 2-4% of all clavicle fractures.
Are there certain populations more at risk for a clavicle fracture?
Although the majority of clavicle fractures are the result of a traumatic event, there are certain groups of individuals that are at a higher risk of experiencing a clavicle fracture. They are as follows:
- Children and Teens. The bones of individuals between the ages of 10 and 19 are still growing and thus have a lower density. These factors make bones more susceptible to fracture.
- Male athletes who participate in contact sports or high-impact activities, such as football, soccer, or wrestling, are three times more likely to experience a clavicle fracture.
- Older Adults. The density of bones decreases with the natural aging process and even minor traumas can result in a clavicle fracture.
What are the symptoms of a clavicle fracture?
A sharp pain of the clavicle immediately following an injury is the most common complaint of a clavicle fracture, although symptoms can vary depending on the severity of the injury. Other common symptoms of a clavicle fracture include:
- Obvious visual deformity of the clavicle
- Pain with arm movement
- Pain, bruising, redness, and swelling of the affected clavicle
- Difficulty with rotating or lifting the affected arm
- Downward shoulder sag
- Shoulder stiffness
How is a clavicle fracture diagnosed?
A comprehensive medical history will be obtained, and Dr. Williams will perform a thorough physical examination. An x-ray of the affected clavicle will be completed to confirm the diagnosis. Additional diagnostic testing, such as magnetic resonance imaging (MRI) scan or CT scan may be requested to rule out any damage to the other structures within the shoulder girdle, and to better understand the morphology of the fractured clavicle.
What is the treatment for a clavicle fracture?
Non-surgical treatment:
If a patient experiences a minor clavicle fracture that did not result in bony displacement, conservative therapies can be effective in resolving symptoms during the healing process. The affected arm will be placed in a sling to keep the clavicle in an acceptable position while healing. A combination of rest, ice, and non-steroidal anti-inflammatory medications (NSAIDs) is recommended for pain and inflammation management. When the pain and inflammation subside, physical therapy is encouraged to restore strength to the shoulder girdle.
Surgical treatment:
Athletic or high demand individuals may be best treated with surgery for clavicle fractures. Clavicle fracture surgery enable the surgeon to achieve anatomic positioning of the affected bone. Shortening of the clavicle after nonoperative treatment may result in anterior displacement of the scapula and chronic posterior shoulder pain. Other circumstances such as failed conservative therapy, a dislocated clavicle, excessive fragment displacement, or open fractures should also be considered for surgical intervention. The clavicle fracture repair (open reduction and internal fixation) procedure utilizes special plates and screws to realign and fix the bone fragments in their proper position.
This procedure is typically done on an outpatient basis using light sedation and regional anesthesia. Most patient will require a sling for approximately two weeks. Home based motion exercises are start immediately following surgery. Formal physical therapy starts approximately one week after surgery. Bony healing usually occurs 6-8 weeks after surgery. Most patients will require some physical therapy for 2-3 months following this procedure to achieve a full recovery.
For more information on clavicle fractures, or the excellent treatment options available, please contact the office of Dr. Riley J. Williams, an orthopedic shoulder specialist serving Manhattan, Brooklyn, New York City, NY and surrounding areas.
Frozen Shoulder Repair Doctor

Have you been diagnosed with adhesive capsulitis or frozen shoulder? If so, you may be eligible for a shoulder treatment called arthroscopic capsular relase. When conservative measures have failed to eliminate shoulder pain and restore range of motion, surgical intervention may become necessary. Doctor Riley J. Williams provides diagnosis as well as surgical and nonsurgical treatment options for patients in Manhattan, Brooklyn, New York City and surrounding areas who have adhesive capsulitis or frozen shoulder. Contact Dr. Williams’ team today!
What is a frozen shoulder?
Frozen shoulder occurs when the connective tissues surrounding the shoulder joint (shoulder capsule) thicken and shorten due to chronic inflammation. This condition is also known as adhesive capsulitis; frozen shoulder causes pain and motion loss in the affected shoulder. In more severe cases, there is a complete loss of shoulder function; simple activities of daily living (hygiene, sleep, dressing, eating) can be difficult and painful.
Frozen shoulder typically has an insidious onset. Although the development of adhesive capsulitis is not completely understood, some underlying health conditions are associated with an increased risk of developing a frozen shoulder. They are as follows:
- A lack of shoulder movement for an extended period, often from a prior injury or surgery, can cause a frozen shoulder.
- Age and sex. A frozen shoulder is more commonly seen in women over the age of 40.
- A frozen shoulder is seen more often in patients with diabetes; these patients typically experience a more severe form of the disease and longer-lasting symptoms.
- Prior surgery to the shoulder girdle or chest area (breast reconstruction).
- Radiation therapy

What are the stages of adhesive capsulitis or frozen shoulder?
There are four stages in the gradual development of adhesive capsulitis:
- Inflammatory phase: characterized by increasing pain with little motion loss. Sleep in difficult.
- Freezing phase: shoulder pain increases resulting in disuse of the affected limb and progression motion loss
- Frozen phase: The affected shoulder is significantly less painful but function is limited because of the motion loss associated with this phase.
- Thawing phase: the patient slowly recovers shoulder motion as the condition wanes.
Most patients will progress through these phases over 2 years without intervention.
What is the treatment for a frozen shoulder?
Patients with a frozen shoulder are generally able to recover with conservative therapy. The goal of conservative treatment is the resolution of shoulder inflammation and the restoration of shoulder range of motion. A combination of rest, ice, and non-steroidal anti-inflammatory medications (NSAIDs) can be used as part of an initial treatment strategy. The judicious use of intraarticular injections of corticosteroids can also be of great value in treating symptomatic adhesive capsulitis patients. Corticosteroids are effective agents that work to decrease the excessive inflammatory process that is characteristic of frozen shoulder joints. Once the inflammation and associated pain have diminished, physical therapy and a home exercise and stretching program are indicated.
What is shoulder arthroscopy with capsular release?
In those circumstances where conservative measures fail to adequately alleviate symptoms, surgical intervention may be necessary to treat the affected shoulder. Surgery for adhesive capsulitis is geared toward removing inflammatory tissues, releasing the shoulder capsule and restoring normal shoulder range of motion. Surgical repair is typically performed at the “freezing” or “frozen” stage of adhesive capsulitis. Frozen shoulder repair is also known as arthroscopic shoulder capsule release. Manual manipulation of the shoulder and an arthroscopic release of the tight ligament around the shoulder are performed together to restore normal shoulder kinematics. Dr. Riley J. Williams, orthopedic shoulder doctor, treats patients in Manhattan, Brooklyn, New York City, NY and surrounding areas, who have experienced a frozen shoulder and need surgical repair.
How is a frozen shoulder surgery/capsular release performed?
The surgery to repair a frozen shoulder is generally performed as an outpatient procedure as an overnight hospital stay is not required for recovery. Prior to the procedure, the patient is sedated and regional anesthesia is administered. Dr. Williams then manipulates the shoulder and carefully moves the shoulder through a sequence of positions to restore range of motion and stretch the inflamed connective tissues. This manual manipulation of the shoulder releases the tight shoulder capsule, improves range of motion of the shoulder, and decreases shoulder pain. Once the manual manipulation is complete, Dr. Williams creates small “keyhole” incisions surrounding the shoulder. A continuous circulation of a sterile solution is introduced into the shoulder joint to enhance visualization of the shoulder joint structures. A small camera (arthroscope) is then inserted through a portal and the images are relayed onto a screen for Dr. Williams to methodically examine the muscles, tendons, and ligaments of the shoulder joint. A radiofrequency probe is then introduced when the shoulder capsule has been identified. This probe uses radiofrequency waves to sever and cauterize the tissue capsule allowing the joint to move more freely. This device is also used to cauterize all inflamed appearing tissues in the shoulder. Once the shoulder capsule has been stretched and released, the arthroscope and surgical instruments are removed, and the incisions are closed with sutures or steri-strips. The shoulder is once again manipulated to confirm the restoration of full passive range of motion of the shoulder joint.
Why is shoulder manipulation important?
Shoulder manipulation under anesthesia as a single operation was the standard procedure for patients with a frozen shoulder. This manual manipulation of the shoulder releases the tight shoulder capsule, improves range of motion of the shoulder, and decreases shoulder pain. When shoulder manipulation was later combined with the arthroscopic capsular release procedure, patients had more successful recovery outcomes.
What are the benefits of arthroscopic capsular release surgery?
Dr. Williams favors the arthroscopic surgical approach as the arthroscope allows for a precise and well-controlled release of the shoulder capsule. The radiofrequency probe implemented in this procedure cauterizes the tissue as it cuts, therefore reducing the bleeding within the joint. Due to the small incisions, this minimally invasive procedure results in a faster recovery period compared to open procedures. Arthroscopic capsular release also minimizes the risk of blood loss and infection as well as decreased pain and inflammation following surgery.
What are the benefits of arthroscopic capsular release surgery?
Dr. Williams favors the arthroscopic surgical approach as the arthroscope allows for a precise and well-controlled release of the shoulder capsule. The radiofrequency probe implemented in this procedure cauterizes the tissue as it cuts, therefore reducing the bleeding within the joint. Due to the small incisions, this minimally invasive procedure results in a faster recovery period compared to open procedures. Arthroscopic capsular release also minimizes the risk of blood loss and infection as well as decreased pain and inflammation following surgery.
For more information on frozen shoulder repair, or to discuss your frozen shoulder treatment options, please contact the office of Riley J. Williams, MD, orthopedic shoulder doctor at the Hospital for Special Surgery (HSS), serving Manhattan, Brooklyn, New York City, NY and surrounding areas.