Shoulder Cartilage Injury Specialist

Are you and athlete who plays contact sports such as hockey or football? Have you experienced a shoulder dislocation? If so, you may be at risk of an articular cartilage injury in the shoulder. Articular cartilage injuries in the shoulder can cause pain, weakness, and loss of range of motion. Articular cartilage injury specialist, Doctor Riley J. Williams provides diagnosis as well as surgical and nonsurgical treatment options for patients in Manhattan, Brooklyn, New York City and surrounding areas who have sustained an articular cartilage shoulder injury. Contact Dr. Williams’ team today!
What is an articular cartilage shoulder injury?
There are three types of cartilage in the body: fibrous, elastic and hyaline. Articular cartilage is a type of hyaline cartilage or tissue found on the ends of bones between joints. Intact articular cartilage facilitates smooth and painless joint motion. It is the most common type of cartilage and can be found between the two main bones that make up the glenohumeral (shoulder) joint. One bone is the scapula (shoulder blade) and the other is the humerus (upper arm bone). Damage to the cartilage in the shoulder can be limited to a focal area; focal areas of shoulder cartilage damage are more common in younger patients. If the damaged area is diffuse (large), it is typically referred to as arthritis, and is more commonly noted in older patients. Cartilage damage often stems from overuse of the joint or from an injury. Injuries may include shoulder dislocation associated with a fall or a direct impact to the shoulder. Dr. Riley J. Williams, orthopedic shoulder specialist, serving Manhattan, Brooklyn, New York City, NY and surrounding areas, has extensive experience in treating articular cartilage shoulder injuries.

What are the symptoms of an articular cartilage shoulder injury?
Individuals in the New York area with articular cartilage shoulder injuries often report the following symptoms:
- Pain and weakness in the shoulder joint
- Clicking, popping, or grinding sensation, mechanical symptoms
- Swelling
- Pain exacerbated by activity or exercise of the shoulder
- Limited range of motion
How is an articular cartilage shoulder injury diagnosed?
Dr. Williams will do a thorough evaluation and assessment. He asks patients questions about their medical history, activity level, symptom duration, and provocative activities that make the pain worse. He will also do a full physical examination of the shoulder and neck. Radiographs of the affected shoulder are almost always part of the examination. If appropriate, a CT scan or MRI is ordered as well. These imaging studies can demonstrate the cartilage damage, and allows Dr. to determine if the issue is focal or diffuse.
How is an articular cartilage shoulder injury treated?
Non-surgical treatment:
Conservative treatment methods are usually the first line of defense for articular cartilage shoulder injuries. An individual may be instructed to rest and ice the shoulder to get the inflammation under control. Excessive joint movement worsen shoulder pain associated with cartilage damage. The use of NSAIDs (non-steroidal anti-inflammatories) can also help manage pain. If these measures do not alleviate the pain, intra-articular corticosteroid, or Platelet Rich Plasma (PRP) injections can be helpful in decreasing shoulder pain due to cartilage damage. Physical therapy focused on improving range of motion and shoulder girdle strengthening are routinely used in patients suffering symptomatic shoulder cartilage injuries. Articular cartilage injuries do not heal on their own, so it is important to follow Dr. Williams’ orders to help prevent further damage.
Surgical treatment:
If non-operative treatments fail, Dr. Williams may suggest surgery to help alleviate the persistent shoulder pain. There are a number of different procedures employed to treat individuals with symptomatic shoulder cartilage damage. Dr. Williams will discuss which surgical option is best suited for treating the problem. These procedures are typically done arthroscopically (minimally invasive) on an outpatient basis. These procedures require the use of small incisions made around the shoulder joint. A small fiber-optic camera (arthroscope) and small surgical tools are used to perform the procedure. Loose pieces of cartilage are removed; areas of focal cartilage damage are smoothed. Any visible inflammatory tissue is removed to decrease joint pain during movement. If cases where the damage to the shoulder is extensive, total shoulder replacement or resurfacing may be indicated.
For more information on an articular cartilage shoulder injury and the treatment options available, please contact the office of Riley J. Williams, MD, orthopedic elbow specialist serving Manhattan, Brooklyn, New York City, NY and surrounding areas.
Suprascapular Nerve Decompression Doctor

Are you experiencing pain and weakness in the back of your shoulder? If so, you may have a shoulder condition called suprascapular neuropathy (SSN) is also called suprascapular nerve entrapment. SSN can cause pain, weakness and eventually nerve dysfunction in your shoulder that requires surgery. Suprascapular nerve decompression can relieve pain and facilitate functional muscle recovery of the shoulder joint. Doctor Riley J. Williams, orthopedic shoulder surgeon, serving Manhattan, Brooklyn, New York City, NY and surrounding areas, has extensive experience in performing suprascapular nerve decompression. Contact Dr. Williams’ team today!
What is suprascapular nerve decompression?
Suprascapular nerve decompression is a minimally invasive surgery performed arthroscopically under regional anesthesia to release pressure on the suprascapular nerve. The suprascapular nerve runs through the scapula (shoulder blade) and sends motor and sensory to the rotator cuff muscles that for movement of the shoulder joint. Compression or pinching of the suprascapular nerve often leads to suprascapular neuropathy (nerve dysfunction). Suprascapular neuropathy present with posterior shoulder pain and weakness noted in the posterior shoulder muscles (infraspinatus and/or supraspinatus muscles). Surgery to decompress a compressed suprascapular nerve can relieve pain and facilitate functional muscle recovery of the shoulder joint. Dr. Riley J. Williams, orthopedic shoulder surgeon, serving Manhattan, Brooklyn, New York City, NY and surrounding areas, has extensive experience in performing suprascapular nerve decompression and other shoulder surgeries.

What is suprascapular neuropathy?
Suprascapular neuropathy (SSN) is also called suprascapular nerve entrapment. The suprascapular nerve originates in the back of the neck and runs through the shoulder blade. This nerve sends sensory and motor signals to the supraspinatus and infraspinatus muscles of the rotator cuff. These muscles move the shoulder joint and the arm. Suprascapular nerve compression is associated with sports that require repetitive overhead arm motion including swimming and volleyball. Direct trauma such as a fall on the shoulder can also cause SSN. Suprascapular neuropathy is a rare injury that occurs in approximately .04% of patients with shoulder pain. Undiagnosed SSN can be a cause of continued shoulder pain after shoulder procedure performed for other shoulder problems including rotator cuff tear, labrum tears and shoulder impingement.
How is suprascapular nerve decompression performed?
The surgery is performed with sedation and regional anesthesia. The procedure is done arthroscopically in an outpatient setting; most patients go home the same day as the surgery. Arthroscopic surgery requires very small incisions at the top and sides of the shoulder. Dr. Williams inserts an arthroscope, which is a fiberoptic viewing lens, and surgical tools in these incisions to complete the procedure. The arthroscope projects images of the shoulder and nerve onto a monitor. Nerve is decompressed is achieved by removing all compressing structures around the nerve (ligaments, cysts). Decompressing the nerve alleviate pains and weakness in the shoulder girdle.
How is suprascapular nerve decompression performed?
The surgery is performed with sedation and regional anesthesia. The procedure is done arthroscopically in an outpatient setting; most patients go home the same day as the surgery. Arthroscopic surgery requires very small incisions at the top and sides of the shoulder. Dr. Williams inserts an arthroscope, which is a fiberoptic viewing lens, and surgical tools in these incisions to complete the procedure. The arthroscope projects images of the shoulder and nerve onto a monitor. Nerve is decompressed is achieved by removing all compressing structures around the nerve (ligaments, cysts). Decompressing the nerve alleviate pains and weakness in the shoulder girdle.
How long does it take to recover?
The patient typically goes home within two hours of the procedure. The arm will be in a sling for approximately a week after the surgery. To rehabilitate the shoulder, physical therapy starts after the first week to help regain range of motion and strength. Most patients should plan to do PT twice a week for 8 weeks. Pain relief is noted soon after surgery; muscle strength recovery may take months to improve after suprascapular nerve decompression.
For additional resources on suprascapular nerve decompression or to have your shoulder pain evaluated, please contact the office of Dr. Riley J. Williams, orthopedic shoulder surgeon serving Manhattan, Brooklyn, New York City, NY and surrounding areas.
Shoulder Bursectomy Doctor

Do you regularly participate in activities that require repetitive overhead arm movements and have subsequently experienced shoulder pain? A condition known as shoulder bursitis is often caused by inflammation from overuse, stemming from constant friction in the shoulder. In severe cases of shoulder bursitis, also called shoulder impingement syndrome, surgery may help alleviate pain and restore function. Shoulder bursitis surgeon, Doctor Riley J. Williams provides diagnosis as well as surgical and nonsurgical treatment options for patients in Manhattan, Brooklyn, New York City and surrounding areas who are experiencing the symptoms of shoulder bursitis or shoulder impingement syndrome. Contact Dr. Williams’ team today!
What is shoulder bursectomy?
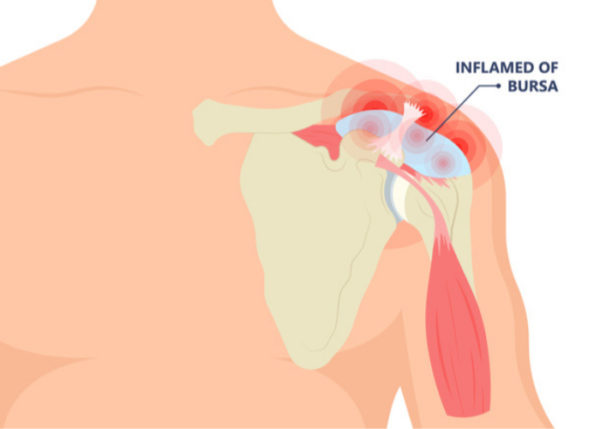
Shoulder bursectomy is arthroscopic surgery that is performed to remove an inflamed bursa. The human body has over 150 bursae that rest between the bone and soft tissues found in many large joints, including the shoulder. There are five main bursae in the shoulder, and when any of these become irritated, it causes inflammation and a condition known as bursitis. The subacromial bursa sits between the top of the rotator cuff and the roof of the shoulder (acromion process). The subacromial bursa can become inflamed by overuse and repetitive overhead arm motion. A shoulder bursectomy is often performed when bursitis persists despite the application of nonoperative treatment modalities. Shoulder bursectomy physically removed the inflamed thickened bursa; this procedure provides patients with pain relief and better shoulder function. When a damaged bursa is removed, a healthy bursal layer grows in its place. Dr. Riley J. Williams, orthopedic shoulder surgeon, serving Manhattan, Brooklyn, New York City, NY and surrounding areas, has extensive experience in performing shoulder bursectomies and other shoulder treatments.
What is bursitis?
Shoulder bursitis or shoulder impingement syndrome occurs when there is an irritation that causes inflammation to the subacromial bursa. The role of bursae is to reduce friction and cushion joints. Increased friction or pathologic overuse can cause the bursa to become inflamed and painful. More severe cases of bursitis can be characterized by an overproduction of fluid and thickening of the bursal tissue. The extra production of fluid can enlarge the bursa; persistent fluid collection associated with bursitis can lead to a predilection toward infection (most commonly in the elbow). Bursitis may be seen in individuals who participate in activities that require repetitive overhead arm movements such as painting, building, swimming, and throwing.
How is a shoulder bursectomy performed?
The surgery is performed under sedation and regional anesthesia; patients typically go home shortly after the procedure on the same day. The procedure is done arthroscopically, which requires two to three small incisions made about the shoulder girdle. An arthroscope is a small camera that’s used to insert in the shoulder to display images of the injury onto a monitor. These images allow Dr. Williams to perform the bursectomy. The inflamed bursa is removed with a small vacuum shaver. If needed, Dr. Williams may remove a small amount of overhanging bone (spur) if he determines that this bony issue was part of what caused the bursitis condition.
What are the risks?
Surgery can come with risks such as blood vessel damage, nerve damage, infection or numbness at the incision sites. Because arthroscopic surgery only requires small incisions, these risks are rare. There is a chance with a bursectomy that an individual may experience pain and a feeling of rubbing or friction in the shoulder joint after surgery until the shoulder fully heals.
How long does it take to recover?
Dr. Williams recommends patients us a sling for 5-7 days following shoulder bursectomy. Physical therapy starts one week after the procedure. Normal activities can be resumed shortly after with pain tolerance as a guide. There are no restrictions or limitations after a bursectomy. A full recovery is anticipated between 2-3 months.
For additional resources on a shoulder bursectomy or to have your shoulder pain evaluated, please contact the office of Dr. Riley J. Williams, orthopedic shoulder surgeon serving Manhattan, New York and the surrounding New York boroughs.
Total Shoulder Replacement Surgeon

Have you been diagnosed with shoulder arthritis? Have conservative measures failed to alleviate your shoulder pain caused by arthritis? If so, you may be a candidate for a total shoulder replacement. Total shoulder replacement surgery is an excellent option for patients suffering from arthritis who have exhausted all non-surgical options. Shoulder replacement surgeon, Doctor Riley J. Williams provides diagnosis as well as surgical and nonsurgical treatment options for patients in Manhattan, Brooklyn, New York City and surrounding areas who have developed shoulder arthritis. Contact Dr. Williams’ team today!
What is total shoulder replacement (Arthroplasty)?
Total shoulder replacement (TSR) is also known as total shoulder arthroplasty. TSR involves replacing the arthritic and damaged surfaces of the shoulder joint using prosthetic implants. The shoulder is a ball and socket joint and is comprised of three bones: the humerus, scapula and clavicle. The humerus is the upper arm bone, and the scapula is the shoulder blade. The superior portion of the humerus (humeral head) along with the glenoid socket of the scapula make up the glenohumeral joint. Total shoulder

replacement is performed on the primary shoulder joint or glenohumeral joint. Articular cartilage lines the end of all long bones and provides the cushion within the shoulder joint, thus allowing the shoulder to move easily and comfortably. Cartilage loss or erosion can occur in association with wear and tear or trauma. Cartilage loss leads to symptomatic arthritis. Cartilage loss results in bone-on-bone contact within the joint, and can cause significant pain and dysfunction. Resurfacing of the humeral head and glenoid socket using the appropriate prostheses as part of the TSR procedure can provide affected patient with durable pain relief and increased function. Doctor Riley J. Williams, Orthopedic Shoulder Surgeon in Manhattan and the New York area, is an expert in performing total shoulder replacement and total shoulder arthroplasty.
Why is total shoulder replacement/arthroplasty performed?
Total shoulder replacement is performed to provide patients with pain relief and increased function. Articular cartilage allows joint surfaces to move fluidly against one another; cartilage is a durable tissue that as a shock absorber. Articular cartilage damage progresses to cartilage loss and exposure of the underlying bone. Joints that are characterized by bone on bone contact are often painful and poorly functioning. Total shoulder replacement enables affected individuals to regain shoulder range of motion of the shoulder and perform normal activities and sports without pain. Degenerative conditions of the shoulder occur following trauma, a fracture, a torn rotator cuff, in association with rheumatoid arthritis (autoimmune) or in association with osteoarthritis (wear and tear). These conditions can lead to significant cartilage loss, joint pain, joint swelling, decreased range of motion and pain.
What is shoulder arthritis surgery?
When conservative treatment methods (rest, corticosteroid injection, physical therapy, NSAIDs, and activity modification) fail to alleviate pain in the arthritic shoulder, TSR may be recommended. There are a few different types of shoulder arthritis surgery that Dr. Williams may suggest depending on the type of injury and age of the patient. These may include:
- Shoulder debridement & synovectomy: Removal of loose bodies and inflamed tissue.
- Total shoulder replacement
Dr. Riley J. Williams, orthopedic shoulder surgeon, serving Manhattan, Brooklyn, New York City, NY and surrounding areas, has extensive experience performing total shoulder replacement and shoulder arthritis surgery.
How is total shoulder arthroplasty performed?
The goal of a total shoulder replacement is to replace the worn and damaged portions of the shoulder with a prosthesis, thus eliminating the pain of osteoarthritis. The humeral head or ball of the shoulder is replaced with a thin metal cover, which is attached to a small stem. This stem is inserted in the proximal humerus bone as a press fit. A high-density plastic prosthesis is used to resurface the socket. Total shoulder replacement is done as an outpatient, and patients can expect to go home the same day. Some patient may wish to stay overnight one night after TSR; Dr. Williams will advise you as to which pathway is best for you based on your medical condition. The surgery is performed with a combination of general and regional anesthesia. Regional anesthesia or nerve blocks help patients with postoperative pain relief. Most patients will not experience pain for several hours after the surgery. Total shoulder replacement surgery takes approximately one hour. Intravenous antibiotics are used before the operation to help limit the chances of infection. Following surgery, patients are advised to use a sling for two weeks.
What are the risks of total shoulder replacement?
Individuals in the New York area who have had total shoulder arthroplasty typically have a very successful outcome. Complication are very rare. TSR surgery has certain risks that may include:
- Infection, although uncommon due to intravenous antibiotics, is possible
- Nerve damage
- Shoulder stiffness
How long is the recovery after a total shoulder replacement?
Once the patient leaves the hospital, his or her arm will be in a sling for two weeks. Absorbable sutures are used, thus removal is not necessary. Dr. Williams will evaluate you two weeks after surgery, subsequent to which, physical therapy will commence. Physical therapy will continue for 2-3 months, twice week. There are daily home exercises that are prescribed to ensure a good outcome. An individual will need to avoid driving for approximately two weeks. A return to normal activities of daily living should be expected by six weeks. Full unfettered recovery takes 4-6 months depending on how quickly the patient is able to restore normal shoulder girdle strength.
For additional resources on total shoulder replacement, shoulder arthritis surgery or to have your shoulder pain evaluated, please contact the office of Dr. Riley J. Williams, MD, orthopedic shoulder surgeon serving Manhattan, Brooklyn, New York City, NY and surrounding areas.
Elbow UCL/MCL Surgeon

Are you an athlete who participates in repetitive overhead movements like tennis or pitching? If so, you are at an elevated risk of tearing the ulnar collateral ligament (UCL), also called the medial collateral ligament (MCL). If an elbow UCL tear is too severe for non-operative treatment, a special UCL repair procedure, called Tommy John surgery, is recommended. Elbow UCL tear surgeon, Doctor Riley J. Williams specializes in Tommy John surgery and the repair or reconstruction of the ULC and MCL in the elbow for patients in Manhattan, Brooklyn, New York City and surrounding areas. Contact Dr. Williams’ team today!
What is UCL or MCL Reconstruction?
Ulnar lateral collateral ligament (UCL) reconstruction is also known as medial collateral ligament (MCL) reconstruction or Tommy John Surgery. This procedure involves surgical repair of a torn ulnar lateral collateral ligament. In most cases, a tendon from the patient’s forearm or leg is used to reconstruct the UCL. UCL reconstruction is an outpatient procedure that is performed under regional anesthesia with sedation. UCL reconstruction is a specialized elbow procedure that is effective at returning affected patient back their normal activities and sports. Dr. Riley J. Williams, orthopedic elbow surgeon, serving Manhattan, Brooklyn, New York City, NY and surrounding areas, has extensive experience in UCL reconstruction/MCL reconstruction/Tommy John surgery.

Why is UCL reconstruction performed?
The ulnar lateral collateral ligament is an elbow stabilizers that protects the joint during throwing and other overhead activities. The UCL attaches the ulna (bone in forearm on the pinky finger side) to the humerus (upper arm bone). The UCL is located on the inner side of the elbow, and is responsible for stability and strength during throwing movements. Repetitive overhand throwing can stress the ligament, weaken it and eventually cause it to tear. Most individuals with a torn UCL will be able to perform activities of daily living, however their ability to throw is significantly compromised. Physical therapy, injection, and bracing do not typically allow affected patient back to their preinjury level of performance, as such, surgery is often the best option for high demand patients with UCL injuries.
Why is UCL or MLC reconstruction referred to as Tommy John surgery?
During the overhand throwing motion, force is applied to the ulnar collateral ligament. Over time, these forces can cause the ligament to fray or rupture; these injuries most often require surgical treatment. UCL injuries are commonly occur in athletes such as baseball players. Tommy John was a pitcher for the L.A. Dodgers in the 1970s. He was one the first professional athletes to undergo UCL surgery; he successfully return to his sport in 1976, two years following the procedure.
How is UCL reconstruction performed?
UCL reconstruction is performed as a same-day surgery; patients go home a few hours after this procedure. Sedation and regional anesthesia are used. During the procedure, Dr. Williams will use a tendon from the patient’s forearm (palmaris tendon) or leg (gracilis tendon) to reconstruct the UCL. After one of these grafts is harvested, an elbow arthroscopy is performed to address any pathology in the elbow joint. The UCL reconstruction requires an incision on the inner elbow. The native ligament is exposed and repaired. The reconstruction is achieved by making small drill holes in the ulna and humerus to facilitate graft passage. Once passed, the graft is tensioned and secure in places using strong sutures. Tommy John surgery takes approximately 60 minutes to complete. Patients return home within a few hours after surgery in an elbow splint.
What are the risks of MCL reconstruction?
Tommy John surgery has a high success rate when completed by an experienced surgeon like Dr. Williams. Individuals may face certain rare risks that include:
- Hematoma
- Ulnar nerve damage
- Re-injury post-surgery
How long does it take to recover from MCL reconstruction?
An individual will leave the hospital after the procedure with their elbow splinted. The splint will stay on for seven to ten days after surgery. The splint is changed to a hinged elbow brace after a week. Range of motion and light strengthening exercises for the arm and shoulder start a week after surgery. At six weeks, the patient can begin exercises to strengthen the elbow. Modified and limited activities for the first four months are essential to ensure proper healing. The interval throwing program starts at month 5. Upper extremity strengthening progresses over several months. Non-throwers can expect a full return to sports around nine months; throwers and pitchers should expect to rehabilitate for a year prior to resuming unlimited sports activities. Patients who follow Dr. Williams’ post-surgical protocol have a high success rate following Tommy John surgery.
For additional resources on UCL reconstruction / MCL reconstruction / Tommy John surgery or to have your elbow pain evaluated, please contact the office of Dr. Riley J. Williams, MD, orthopedic elbow surgeon serving Manhattan, Brooklyn, New York City, NY and surrounding areas.