Dr. Riley Williams was recently highlighted for his surgical skills, repairing an ACL.
In this video, courtesy of CNN, Meredith Speck, a patient of Dr. Williams, is part of a growing list of female sports athletes who are sustaining ACL injuries on the soccer field. Dr. Williams was proud to be featured in this video (at :39) performing her ACL operation.
Women’s Soccer is one of the sports that has all the makings of an ACL injury waiting to happen, especially in females since they are 3-4 times more likely to experience this injury than their male counterparts.
Why are women more susceptible to ACL tears?
Here are a few reasons, outlined in the video:
-
Hormones:
- Female hormones, such as estrogen, progesterone and relaxin can all have an effect on the laxity, or stretchiness of all ligaments in the body, not just in the knee. For female soccer players, this becomes important because the looser the ligament, the more likely it is to stretch under pressure, this limits the stability of the knee and can allow the tibia to slide out in front of the femur.
-
Femoral Notch:
- The femoral notch, where the ACL is located, is genetically more narrow in females and in males. This narrow space makes the ACL more prone to injury because the knee ligament can be pinched between the femur and the tibia.
-
ACL is Smaller:
- Men genetically have a larger, stronger ACL
-
Greater Q-Angle:
- A greater Q-Angle (as shown in the video) allows almost a knock-kneed appearance for women, which makes the ACL more vulnerable to injury.
How can women help prevent an ACL injury or tear?
Strengthening and conditioning in the correct way is important in keeping a healthy ACL. As the video shows, a focus on strengthening the hip and thigh muscles can provide stability to the knee and prevent injury. Body mechanics are also an important aspect of a healthy knee, especially when learning to land, pivot or change directions. Finally, a proper warm up and cool down period can help keep the knee and its surrounding muscles in good health.
What is the difference between ACL repair and ACL reconstruction?
Anterior cruciate ligament (ACL) injuries are a significant clinical problem for individuals who participate in pivoting sports (i.e. soccer, lacrosse, American football, basketball, downhill skiing, tennis, pickleball). Knee instability associated with an ACL tear may predispose patients to meniscal injuries, cartilage damage, and eventually osteoarthritis.
The current gold standard in the treatment of ACL injuries is ACL reconstruction. ACL reconstruction utilizes an alternative ligament or tendon source to replace the injured ACL.
Primary ACL repair is currently a hot topic in Orthopedic Surgery and Sports Medicine. It is important for the ACL-injured patient to have a solid understanding of the benefits, outcomes, and risks of a repair vs a reconstruction as they decide how best to treat their specific injury. Doctor Riley J. Williams provides diagnosis as well as surgical and nonsurgical treatment options for patients in Manhattan, Brooklyn, New York City and surrounding areas who need an expert repair or reconstruction of their ACL.

What is primary ACL repair?
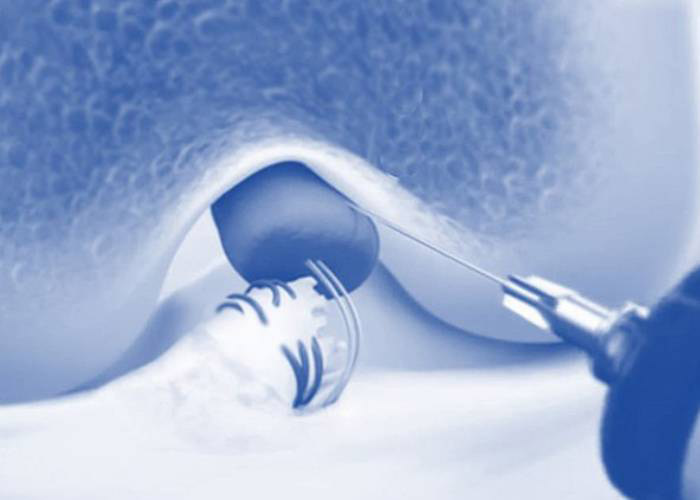
Primary ACL repair involves suturing the torn ACL back together. ACL repair does not utilize a donor graft source. The torn ends of the ACL are trimmed to remove any frayed or damaged tissue, carefully aligned, and sutured together. Alternatively, the torn ACL may be reattached to the bone on which it naturally inserts using sutures and bone tunnels., ACL repair configurations may be reinforced, synthetic scaffolds, biological adjuncts, or other external devices.
Why is there recent renewed interest in primary ACL repair?
Advancements in surgical techniques and technologies have made primary ACL repair more feasible. ACL repair was thoroughly studied in the 1980s and replaced with more modern and effective ACL reconstruction techniques. Surgeons who recommend the ACL procedure as an alternative to ACL reconstruction point out the potential for a shorter recovery time, the idea of preserving a patient’s natural ligament tissue and reduced risk of donor site morbidity as the procedure does not involve harvesting donor tissue graft. Moreover, offering patients the option of ACL repair is also a way for Orthopedic Surgeons to differentiate themselves from other knee surgeons.
Does primary ACL repair have a lasting positive outcome?
While primary ACL repair can be a viable option for a small subset of patients with ACL tears, it is not suitable for most patients, especially those patients who actively participate in pivoting sports. The clinical success rates of the ACL repair are inferior to ACL reconstruction; moreover, revision rates of ACL repair patients far exceed those observed for ACL reconstruction patients. Failure rates of ACL repair procedures are especially high in young patients (age less than 30 years) who participate in ballistic, high demand sports. Patients considering primary ACL repair should seek a second opinion from an orthopedic surgeon who specializes in the treatment of ACL injuries to confirm the appropriateness of ACL repair in their specific circumstance.
Doctor Williams’ practice specializes in the treatment of knee ligament injuries; he performs a high volume of both primary and revision ACL surgeries. Unfortunately, many of these revision ACL surgeries are performed on patients who underwent primary ACL repairs from other practices. ACL repair does have a place in the continuum of ACL treatment options following ACL injury. It is a reasonable option in lower demand, older patients.
Facts about primary ACL repair surgery?
- Primary ACL repair is typically only considered for patients with a proximal (femoral) avulsion tear (the ligament is pulled away from the bone); other tear configurations (i.e. mid-substance) are less optimal for current ACL repair methods.
- Suturing a torn ACL back without causing additional damage to the ligament requires a high level of surgical skill and expertise, making it potentially more challenging than ACL reconstruction surgery.
- The success rates of primary ACL repair are generally poorer than those of ACL reconstruction, particularly for athletes or individuals with high activity levels. The repaired ACL is more prone to re-tearing and may not provide the same stability as a reconstructed ACL.
- While a shorter recovery time is often one of the benefits touted for primary ACL repair, the recovery time is often actually longer than after ACL reconstruction because the repaired ACL needs time to heal and regain strength. Oftentimes, ACL repair patients must be immobilized early in the rehab process to facilitate ligament healing. This can result in knee stiffness and loss of leg strength.
- The long-term results and durability of current ACL repair methods are unknown.
Is primary ACL repair less expensive than ACL reconstruction?
ACL repair is not less expensive than ACL reconstruction.
Does primary ACL repair surgery take less time than ACL reconstruction?
No. Skilled ACL surgeons should be able to complete a primary ACL repair or ACL reconstruction in under an hour.
What is the take home message for ACL repair vs reconstruction?
Although ACL repair is an emerging approach in the treatment of the ACL injured patient, clinical results and revision rates of primary ACL repair are inferior to ACL reconstruction. Patients should consult with a surgeon well-versed in the treatment of these injuries before moving ahead with either ACL repair or ACL reconstruction.
ACL Tear Repair or Reconstruction Surgeon

If you participate in pivoting sports, or in activities that involve jumping or quick stopping, you are at risk of injuring or tearing your ACL (anterior cruciate ligament) in your knee. The decision to repair or reconstruct the ACL depends on a lot of different factors and varies per individual. Patients who want to return to sport should weight their options carefully. ACL surgeon, Doctor Riley J. Williams provides diagnosis as well as surgical and nonsurgical treatment options for patients in Manhattan, Brooklyn, New York City and surrounding areas who have sustained an ACL injury. Contact Dr. Williams’ team today!
What is Bridge-Enhanced ACL Repair (BEAR)?
Bridge-Enhanced ACL Repair (BEAR) is a surgical technique that uses a special sponge-like scaffold to encourage the healing of the injured Anterior Cruciate Ligament (ACL). This procedure is considered an adjunct to primary ACL repair. This specific procedure involves placing a scaffold, derived from cow (bovine) tissue, across the torn ends of the injured ACL. The scaffold is in place by sutures and acts as a healing bridge while the torn ends of the ligament attempt to grow back together and heal. Doctor Riley J. Williams provides diagnosis as well as surgical and nonsurgical treatment options for patients in Manhattan, Brooklyn, New York City and surrounding areas who need expert advice regarding the BEAR Repair.
Gunter Sokoi, CC BY-SA 4.0, via Wikimedia Commons
When is Bridge-Enhanced ACL Repair (BEAR) recommended?
The BEAR implant is an experimental treatment. The BEAR may be recommended as an alternative to traditional ACL reconstruction for patients with partial or complete tears of the ACL who are between the ages of 14 and 35 and have not undergone previous ACL surgery. The procedure may also be performed within a few weeks of the injury.
How long has Bridge-Enhanced ACL Repair (BEAR) been available?
BEAR’s testing in human patients began with a preliminary clinical trial several years ago. Since then, a number of larger clinical trials have been conducted. The long durability of patients treated with ACL repair and the BEAR implant is unknown.
Why is Bridge-Enhanced ACL Repair (BEAR) recommended instead of ACL reconstruction?
In contrast to traditional ACL reconstruction surgery that involves harvesting a donor graft to replace the injured ACL , the BEAR procedure features a scaffold that encourages the body to primarily heal the torn ligament. The procedure BEAR is performed on an outpatient basis. The surgery itself is slightly less invasive compared to traditional ACL reconstruction. The BEAR is considered an adjunct to primary ACL repair.
What are the risks of Bridge-Enhanced ACL Repair (BEAR)?
The biggest risk of Bridge-Enhanced ACL repair is the increased risk of graft failure compared to traditional ACL reconstruction. Patients who regularly participate in higher demand pivoting sports should consider this when selecting a treatment strategy for their ACL surgery.
Otherwise, the BEAR procedure carries the same risks as most surgeries, including infection, bleeding, nerve damage, and blood clots.
What is the success rate of Bridge-Enhanced ACL Repair (BEAR)?
The success rate of BEAR is dependent on several factors including the extent of the ACL tear, the age of the patient, and the level of physical activity. Clinical studies have shown that the procedure has a success rate of approximately 80% . There is concern about the use of this methodology in young athletes who play pivoting sports (basketball, soccer, lacrosse, football, downhill skiing, gymnastics).
The Bridge-Enhanced ACL Repair (BEAR) procedure is a relatively new option in the treatment of ACL injuries. More clinical studies are needed to ensure the long-term durability and clinical success rates of primary ACL repair using the BEAR implant. Currently the clinical outcomes of the BEAR procedure do not match those observed with traditional ACL reconstruction surgery.
BEAR – Bridge-Enhanced ACL Repair Surgeon

Bridge-Enhanced ACL Repair (BEAR) is a new(er) surgical method of repairing an ACL that features a scaffold which encourages the body to primarily heal the torn ligament. The BEAR method is not the best procedure for some patients and it is best to talk with an expert to see if this would be the best treatment for your torn ACL. ACL surgeon, Doctor Riley J. Williams provides diagnosis as well as surgical and nonsurgical treatment options for patients in Manhattan, Brooklyn, New York City and surrounding areas who have sustained an ACL injury. Contact Dr. Williams’ team today!

Telehealth/Virtual Consultations and/or Second Opinion with Dr. Williams
Dr. Williams offers virtual second opinions, consultations, and imaging reviews. His partnership with “Best In Class MD” (BICMD) allows Dr. Williams to provide a comprehensive service that includes a thorough review of your medical records and imaging. You will receive written recommendations and a treatment plan outline in his Expert Report. This service is especially helpful for out-of-state or internationally located patients seeking an expert consultation.
Telehealth is also helpful for patients who need an immediate consultation or do not have time to wait for an in-person appointment.
It’s easy:
To set up a remote second opinion or imaging review, please click the link below to schedule an appointment.
The BICMD care team is available to answer any questions about booking at [email protected] or 800-650-5907.
Are you located in the New York City area and would rather go through your insurance?
Dr. Williams can still provide a telehealth visit with you! All you need is a smart phone or webcam so that he can assess your orthopedic condition and offer the best treatment options. Click the link below to schedule an in-person or telehealth that is covered by your insurance.
Dr. Williams speaks at the Isokinetic Medical Group Conference
After two long years, the Isokinetic Medical Group Conference was finally able to gather in person again!
Last weekend, June 4 – 6, 2022, Riley Williams spoke in Barcelona Spain.
The theme this year was: Football Medicine: The Players’ Voices
Dr. Williams provided insight on articular cartilage repair in the high demand athlete.
About the Isokinetic Medical Group:
Isokinetic is a specialist Sports Medicine and Rehabilitation Group, recognized as FIFA Medical Centre of Excellence, and a reference point in the orthopaedic and sports rehabilitation sectors.
About two hundred people work together in the Isokinetic network, sharing the same values and acting as a team, with the common goal, since 1987, to seek daily excellence on the patient and with the commitment to provide the best possible care.
A group that consistently benchmarks the results of its work, both internally within the network as well as with the international medical community. The power of innovation is found in the strategic positioning of its “Education and Research Department” at the heart of the Isokinetic system.