Knee Osteochondritis Dissecans (OCD) Specialist

Are you a young athlete who participates in high impact sports with continuous jumping or running? If so, you may be at risk for a rare condition known as osteochondritis dissecans of the knee (OCD). Knee OCD specialist, Doctor Riley J. Williams provides diagnosis and both surgical and nonsurgical treatment options for patients in Manhattan, Brooklyn, New York City and surrounding areas who are experiencing symptoms associated with knee OCD. Contact Dr. Williams’ team today!
What is OCD of the knee?
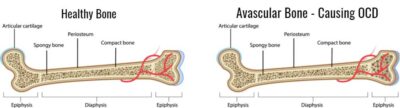
Osteochondritis dissecans is a musculoskeletal condition that characterized by the presence of a focal area of dead bone beneath the articular cartilage of an affected joint. It is thought that the bone death noted in OCD lesions is due to a lack of blood flow during the embryonic development. Despite being a congenital condition, most patient do not experience symptoms associated with an OCD lesion until the 2nd or 3rd decade of life. OCD lesions can cause pain. In cases where the cartilage over the OCD lesions breaks off, mechanical symptoms and knee joint locking can occur. OCD lesions are a type of osteochondral lesion or defect.
There are two types of OCD: adult and juvenile (JOCD). The cause of OCD is unknown but is more likely to occur in the male population. The cause of JOCD is believed to stem from repetitive stress to the knee due to sports and microtraumas to the knee. Dr. Riley J. Williams, orthopedic knee specialist, serving Manhattan, Brooklyn, New York City, NY and surrounding areas has extensive experience in treating osteochondritis dissecans lesions (OCD) of the knee and other knee deformities.
Who is typically affected by OCD lesions?
Adolescents and young adults are most typically affected by OCD lesions. Athletic activities can increase symptoms in these patients. OCD occurs most commonly in the knee, but can also occur in ankles, elbow, shoulder and other joints.
How are OCD lesions characterized?
Osteochondritis dissecans lesions are staged according to their size and state of attachment. Stable lesions are those where the cartilage over the abnormal bone remains intact. Unstable lesions describe those where the cartilage over the abnormal bone is partially or completely detached. Stable lesions, when symptomatic, usually cause achiness and pain. Unstable lesions are usually notable for the knee joint locking and catching associated with the loose cartilage fragment. Dr. Riley J. Williams, orthopedic knee specialist serving Manhattan, Brooklyn, New York City, NY and surrounding areas has extensive experience in diagnosing and treating knee osteochondritis lesions.
What are the symptoms of osteochondritis dissecans (OCD) of the knee?
Adult and adolescent patients typically experience the same symptoms and knee pain is localized to the area where the OCD exists. Knee pain may worsen with normal daily activities or sports. Specific symptoms may include:
- Mild to moderate, aching pain that progressively gets worse
- Tenderness or achiness
- Swelling
- Locking of the knee or mechanical catching of the knee
- Loose body movement within the knee
- Pain while bearing weight
Is OCD (Osteochondritis Dissecans) the same thing as an osteochondral defect?
Osteochondritis Dissecans (OCD) is a type of osteochondral defect. The two clinical conditions are closely related. Osteochondritis Dissecans and osteochondral defects can occur in any joint, but frequently occur in the knee joint. OCD lesions are characterized by an area of abnormal bone (dead or necrotic bone) that lies below an area of normal cartilage. Over time, the cartilage over this area of abnormal bone starts to detach or collapse because the underlying bone is soft and abnormal. Most OCD lesions are present at birth; symptoms associated with OCD lesions typically occur in the second to third decades of life. The exact cause of OCD lesions is unknown; OCD lesions are thought to be caused by micro-traumas to the knee that occur in utero. OCD lesions are congenital. Although OCD lesions are a type of osteochondral defect, there are other types of osteochondral lesions that involve damage to the articular cartilage and can affect the underlying bone. The distinction between the two conditions is the congenital nature of osteochondritis dissecans, and the abnormal bone of OCD that ultimately results in an overlying cartilage lesion. Many physicians will use these two terms interchangeably.
How are OCD lesions of the knee diagnosed?
It is not unusual for an OCD lesion to go undiagnosed for years. Dr. Riley J. Williams will ask the patient about his or her history of pain. Dr. Williams will perform a physical examination to determine the affected area on the knee. Radiographs are used to help determine if an OCD lesion is present. Dr. Williams will order an MRI Scan to diagnose and better visualize the OCD lesion. The MRI will show him the articular cartilage surfaces. The MRI scan will allow Dr. Williams to determine the size, shape and progression of the injury. He will be able to determine the amount of bone damage and will formulate a plan for treatment and repair of the defect.
What is the treatment for OCD of the knee?
Treatment for this type of knee injury or defect will vary, based on the patient’s activity level and on the size, location and amount of damage caused by the defect.
Non-surgical treatment:
The goal of conservative treatment is to reduce pain associated with the OCD defect. The mainstays of nonoperative treatment are rest, activity modification, bracing, physical therapy and non-steroidal anti-inflammatory medication, such as ibuprofen or naproxen. Younger patients (skeletally immature) may experience a resolution of symptoms after the knee growth plates have closed.
Surgical treatment:
Surgical treatment for osteochondritis dissecans lesions is necessary if the lesion continues to be painful despite conservative treatment or if the lesion detaches from the knee condyle or patella. Dr. Williams may need to repair or remove the detached fragment. He can gain understanding of the necessary surgery by first using an arthroscope, which is a very small camera, inserted into the knee. He then uses small, specialized instruments to perform the surgery within the knee. Treatments may include:
- Arthroscopic knee debridement will remove loose bodies in the knee and can smooth down rough or torn tissue.
- Pinning of the OCD fragment involves stabilizing the loose OCD fragment with pins or screws to promote healing of the affected area
- Autograft osteochondral transplant (mosaicplasty)
- Allograft transplant obtained from a donor or cadaver can replace damaged cartilage tissue.
- Osteochondral autograft uses tissue obtained from the patient to restore the damaged bone and cartilage.
- Autologous chondrocyte implantation uses the bodies own cartilage cells, which are removed, grown in a lab, and implanted in the knee. The new cartilage that is grown from the cells is used as a patch replace the damaged area.
- Particulate juvenile articular cartilage obtained from donors can be used to regrow missing cartilage due to a detached OCD lesion
- MACI – Matrix Associated Autologous Chondrocyte Implantation
- Stem Cell Therapy
Patients should not bear weight on the injured knee after surgery. Physical therapy, strengthening exercises or a continuous passive motion machine, which is a machine that gently moves your joint to prevent stiffness, may be required.
For more information on osteochondritis dissecans lesions (OCD) of the knee and the treatment options available, please contact the office of Riley J. Williams, MD, orthopedic knee specialist serving Manhattan, Brooklyn, New York City, NY and surrounding areas.
Locations
610 W 58th Street
New York, NY 10019
148 39th Street, 7th Floor
Brooklyn, NY 11232