Objectives: Osteochondral autograft transfer (OAT) and fresh osteochondral allograft transplantation (OCA) are popular cartilage restoration techniques that involve the single-stage implantation of viable, mature hyaline cartilage into focal chondral defects of the knee. Both techniques have demonstrated good results, as defined by statistically significant post-surgical improvements in patient-reported outcome measures. Recently, there has been greater focus on what represents a clinically relevant change in outcomes reporting, and commonly applied metrics for measuring clinical significance, such as the minimal clinically important difference (MCID) and substantial clinical benefit (SCB), have become the standard. Although a previous study defined a MCID in patients treated for articular cartilage defects in the knee (Greco et al, AJSM 2010), these patients were treated with various cartilage restoration procedures (e.g., debridement, microfracture, autologous chondrocyte implantation), and none were treated with OAT/OCA. Therefore, the purpose of this study was to define the MCID and SCB thresholds after OAT/OCA for the International Knee Documentation Committee subjective knee form (IKDC) and Knee Outcome Survey-Activities of Daily Living Scale (KOS-ADL) and to determine clinical and demographic patient factors predictive for achieving the MCID and SCB after OAT/OCA.
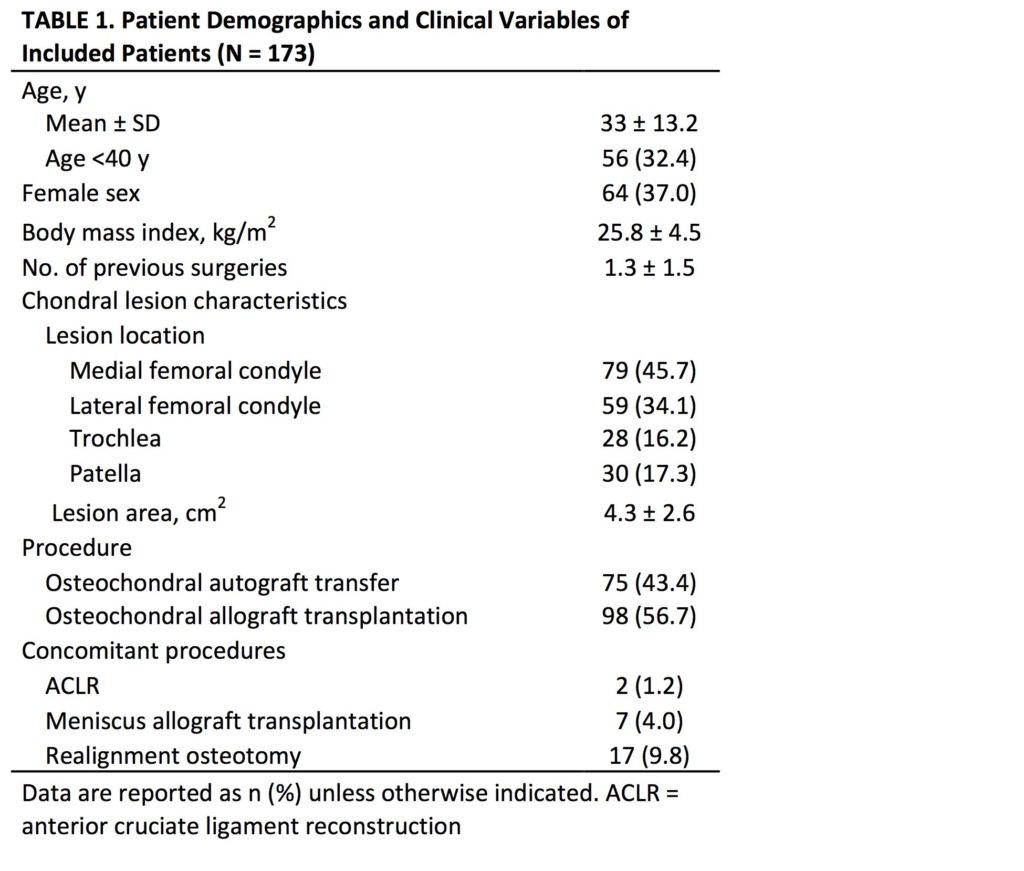
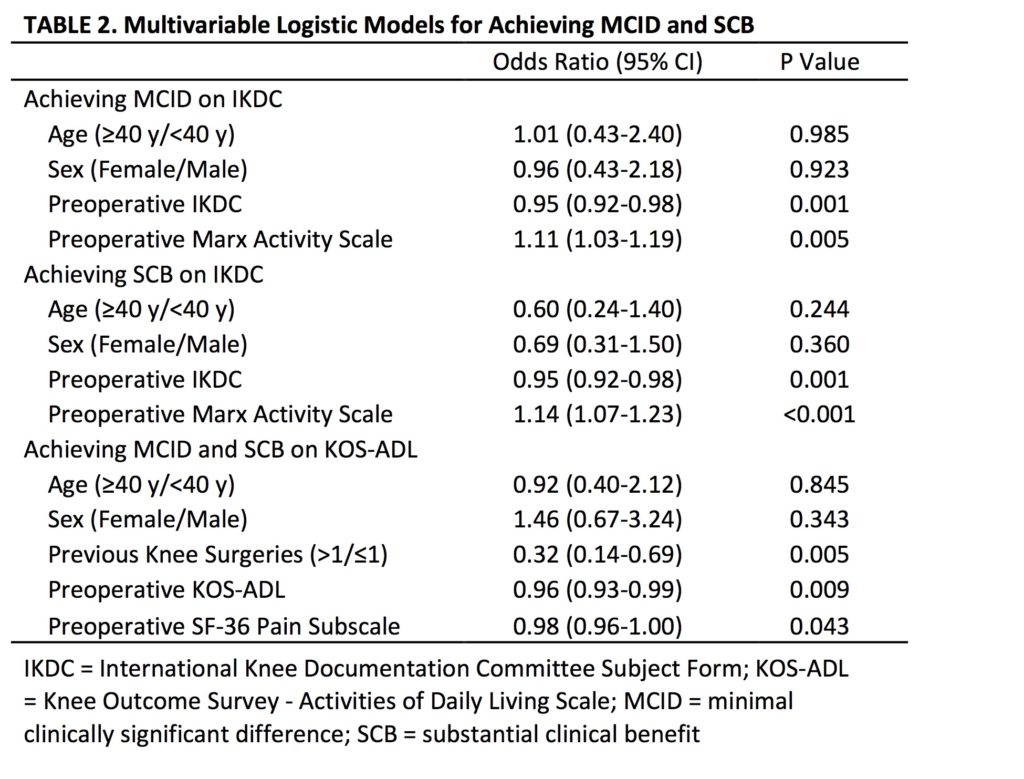
Methods: A prospective institutional cartilage registry was reviewed to identify patients who underwent OAT/OCA. The IKDC and KOS-ADL were administered preoperatively and at a minimum of 2 years postoperatively. The MCID and SCB of these outcome scores were calculated using anchor-based methods. Receiver operativecharacteristic (ROC) analysis was used to determine the SCB using an anchor question, with the area under the curve (AUC) used to evaluate predictive ability. Multivariate analysis was performed to identify patient factors associated with achieving the MCID and SCB. Results: In total, 173 knees in 173 patients (mean age, 33.0 ± 13.2 years; 37.0% female) were identified. Patient demographics and clinical variables are listed in Table 1. Using the anchor-based method, the MCID for the IKDC and KOS-ADL were 17 ± 3.9 and 10 ± 3.7, respectively. Using the ROC method, the SCB for the IKDC and KOS-ADL were 32 (AUC 0.86) and 10 (AUC 0.76), respectively. Univariate analysis demonstrated no association between procedure (OAT or OCA) or lesion location and likelihood of achieving the MCID/SCB. In multivariate analysis, lower preoperative IKDC scores and higher preoperative Marx Activity Scale scores were predictive of achieving an MCID and SCB on the IKDC, and lower preoperative KOS-ADL scores, lower preoperative SF-36 pain subscale scores, and a history of 1 or less previous ipsilateral knee surgeries were predictive of achieving a MCID and SCB on the KOSADL (Table 2).
Conclusion: In patients treated for focal cartilage defects of the knee with osteochondral grafts, these values can be used to define a clinically important change and substantial clinical benefit for future outcome studies. In this study population, higher preoperative activity levels and a history of 1 or less previous ipsilateral knee surgeries were predictive of achieving a clinically important change and substantial clinical benefit after OAT/OCA. These findings have implications for managing preoperative expectations of OAT/OCA surgery
Read Full Article (via SAGE Journals)